Medicaid Generic Coverage: State-by-State Variations and Requirements
 Jan, 10 2026
Jan, 10 2026
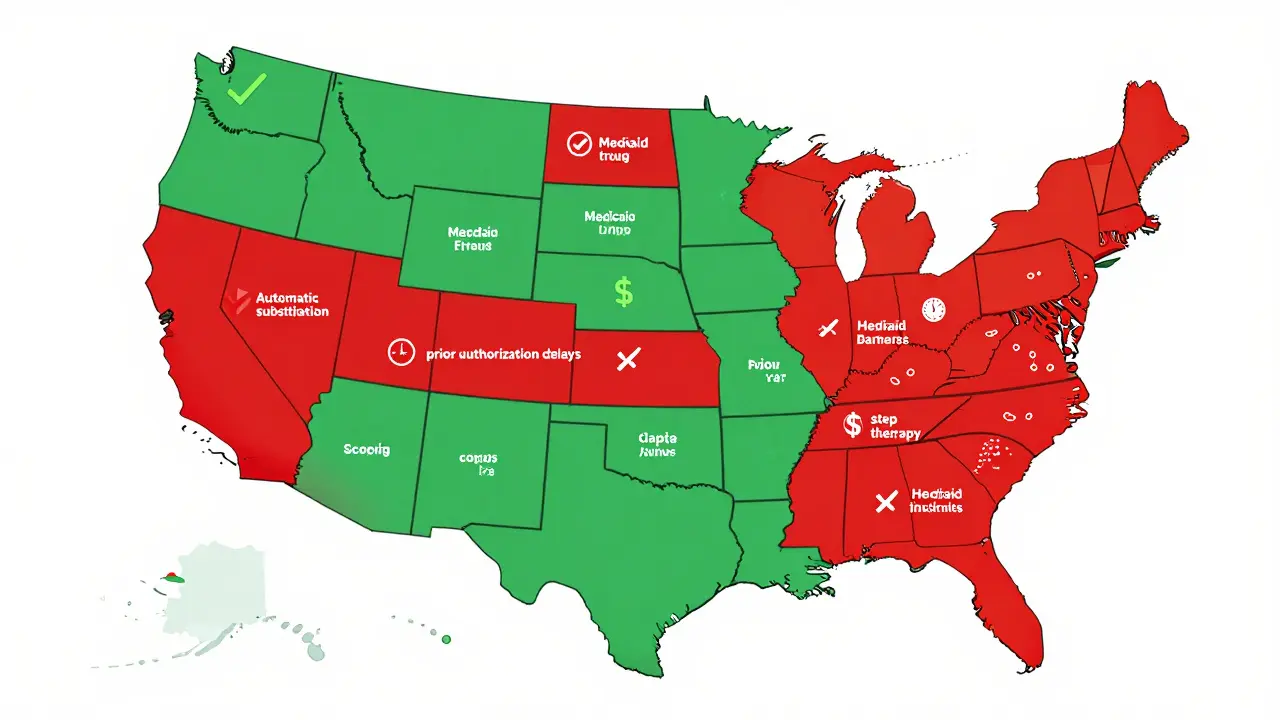
When you're on Medicaid, getting your generic prescriptions shouldn't be a maze-but in reality, it often feels like one. What’s covered, how much you pay, and whether you need prior authorization all depend on which state you live in. Even though every state offers prescription drug coverage under Medicaid, the rules for generic drugs vary wildly. One state might automatically swap a brand-name pill for its generic version without a second thought. Another might require you to try three other drugs first, pay $8 out of pocket, and wait three days for approval. This isn’t just paperwork-it affects whether someone takes their blood pressure medicine, insulin, or asthma inhaler every day.
How Medicaid Generic Coverage Works (Federal Baseline)
All 50 states and Washington, D.C., cover outpatient prescription drugs under Medicaid. That’s not optional-it’s how the program works today. But the federal government doesn’t dictate the details. Instead, it sets the floor: any drug from a manufacturer enrolled in the Medicaid Drug Rebate Program must be covered, unless it’s on the federal exclusion list. That list includes drugs for fertility, weight loss, erectile dysfunction, and cosmetic purposes. Beyond that, states have near-total control. The real engine behind generic drug pricing is the Federal Upper Limit (FUL). CMS calculates this every month, setting the maximum amount Medicaid will pay for a generic drug. It’s based on 150% of the average manufacturer price plus a small fee. States can set lower limits, and most do. That’s why a generic version of metformin might cost $4 in one state and $1 in another. The lower the FUL, the more the state saves-but it also means pharmacies might be less willing to participate if reimbursement is too tight.Automatic Generic Substitution: Not Everywhere
At least 41 states require pharmacists to substitute a generic drug when it’s available and therapeutically equivalent to the brand-name version. That sounds straightforward-until you dig into the exceptions. In Colorado, for example, the law says a generic must be dispensed unless the prescriber writes "dispense as written" or the brand drug is actually cheaper. That’s rare, but it happens. In other states like California, substitution is automatic unless the patient objects. But in some places, pharmacists need to notify the doctor before switching, even if the drugs are identical. Twenty-eight states require documentation of therapeutic equivalence, while 12 let pharmacists switch without telling anyone. That inconsistency creates confusion for patients and providers alike.Formularies and Tiers: What’s Covered and What’s Not
Every state runs a Preferred Drug List (PDL), which organizes medications into tiers. Tier 1 is almost always generics. Tier 2 is brand-name drugs. Some states have Tier 3 for specialty generics. But here’s the catch: just because a drug is on the list doesn’t mean it’s easy to get. Take CVS Caremark’s 2025 Medicaid formulary. It lists hundreds of generics in Tier 1. But each state picks which drugs from that list they’ll cover-and whether they’ll require step therapy. That means you might have to try two cheaper generics before the system will pay for the third, even if your doctor says you need it. Thirty-two states use step therapy for drugs like antidepressants, diabetes meds, or arthritis treatments. In Colorado, you might need to fail three NSAIDs and three proton pump inhibitors before they’ll approve a more expensive GI drug. In Massachusetts, the process is simpler. The difference isn’t just policy-it’s whether someone sticks with their treatment.
Prior Authorization: The Hidden Barrier
Prior authorization is the biggest headache for patients and doctors. It’s not just for expensive drugs anymore. In many states, even common generics like gabapentin or metoprolol require pre-approval. Health First Colorado requires prior authorization for non-preferred drugs, and some medications-like opioids-have extra rules: 7-day supply limits, 8 pills per day max. Other states, like Texas, have fewer restrictions on generics but longer wait times. Decisions can take 24 hours in some states, up to 72 in others. That delay can mean skipped doses, ER visits, or hospitalizations. A 2024 University of Pennsylvania study found that when Medicaid patients had their generic prescriptions denied, hospital admissions jumped by 12.7%. Primary care doctors spend an average of 15.3 minutes per patient just handling prior auth requests. That’s over $8,200 a year in lost time per physician. It’s not just a cost to the system-it’s a cost to care.Copays: How Much You Pay Out of Pocket
Medicaid beneficiaries with income under 150% of the federal poverty level can be charged copays for non-preferred generics-up to $8 per prescription. Most states charge less: $1 to $4 is common. But even $4 adds up. If you’re taking three generics a month, that’s $12 a month. For someone living paycheck to paycheck, that’s food or rent money. Some states, like Vermont and Minnesota, charge $0 copays for all generics. Others, like Mississippi and Alabama, charge the full $8. There’s no national standard. And it’s not always clear which drugs are considered "preferred"-that list changes every quarter. Patients often find out they owe money only when they get to the pharmacy counter.Pharmacy Access: Not All Pharmacies Are Equal
Even if your drug is covered and you’ve gotten prior auth, you still need a pharmacy that accepts Medicaid. And not all do. In Vermont, 98.2% of community pharmacies participate in Medicaid. In Texas, it’s just 67.4%. Why? Reimbursement rates. If Medicaid pays too little, pharmacies lose money on every generic dispensed. Many small, rural, or independent pharmacies simply can’t afford to stay in the network. That leaves patients driving farther, waiting longer, or skipping doses. And it’s not just about location. Some PBMs-like CVS Caremark, Express Scripts, and OptumRx-manage pharmacy benefits in 37 states. That means you might get different rules depending on who runs your benefits, even within the same state.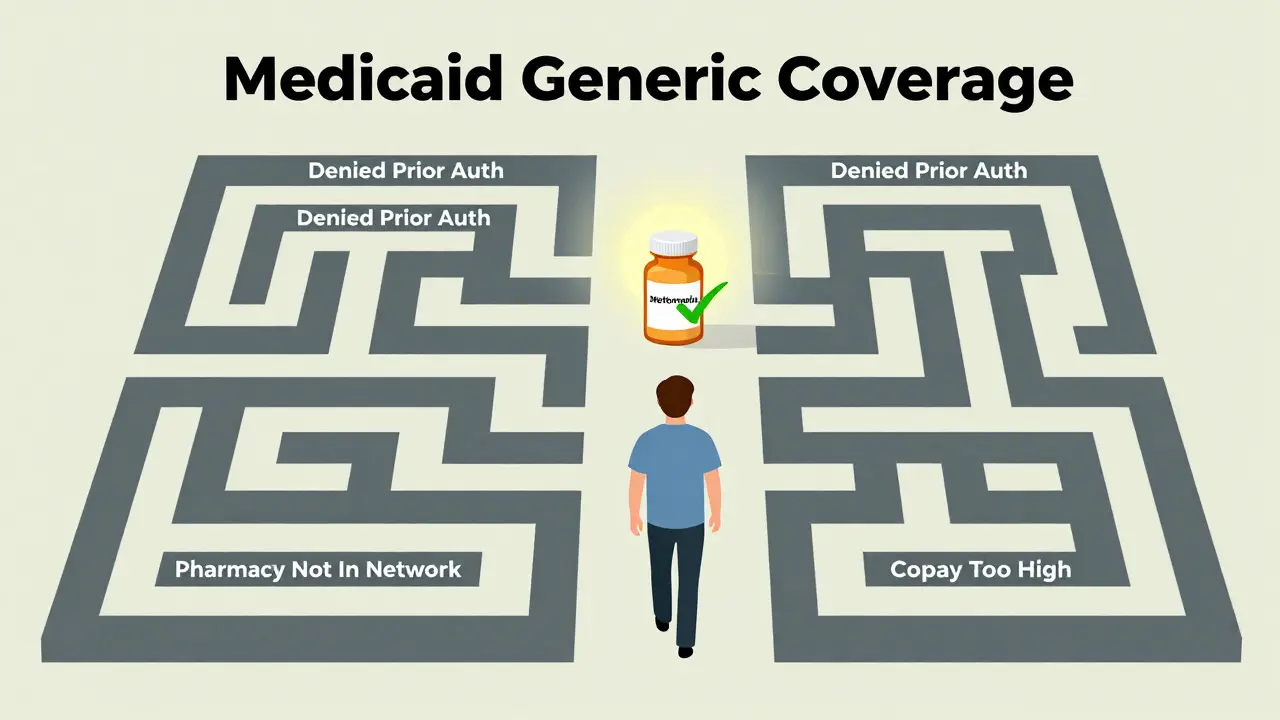
What’s Changing in 2025 and Beyond
New rules are coming. In late 2024, CMS proposed requiring Medicaid to cover anti-obesity medications like semaglutide. If approved, that would be the biggest expansion of covered drugs since the Affordable Care Act. But it’s controversial. States worry they’ll be stuck paying for drugs without enough federal funding. There’s also a proposed law that would remove most generic drugs from the Medicaid Drug Rebate Program’s inflation-based rebates. If that passes, states could lose an estimated $1.2 billion a year in rebates. That could mean higher copays, tighter formularies, or even drug exclusions. Meanwhile, the Medicare Two Dollar Drug List Model-though discontinued-showed something important: when generics are priced at $2 or less, adherence goes up by nearly 18%. States are watching. Michigan’s pilot program for diabetes generics cut costs by 11% while keeping patients on their meds. That’s the kind of model others want to copy.What Patients Should Do
If you’re on Medicaid and taking generics:- Ask your pharmacist: "Is this drug on my state’s preferred list?"
- Call your state Medicaid office for the latest formulary-don’t rely on your doctor’s memory.
- If you’re denied a drug, file an appeal. Many denials are overturned.
- Check if your state offers a mail-order pharmacy program. It often has lower copays.
- Keep a list of your meds and any prior auth approvals. Changes happen fast.
What Providers Should Know
Doctors and nurses need to stay updated on state-specific rules. A drug approved in New York might be denied in Georgia. Use your state’s online formulary lookup tool-most are free and updated monthly. Don’t assume a generic is automatic. Always check:- Is prior auth required?
- Is step therapy needed?
- What’s the copay?
- Is the pharmacy in-network?
Do all states cover generic drugs under Medicaid?
Yes. All 50 states and Washington, D.C., cover outpatient prescription drugs, including generics, for eligible Medicaid enrollees. While federal law makes pharmacy coverage optional, every state has chosen to include it as part of their program.
Why do copays for generic drugs vary so much between states?
States can set copays up to $8 for non-preferred generics for low-income beneficiaries, but many choose lower amounts or $0. The variation comes from budget priorities, pharmacy reimbursement rates, and political decisions. States with higher Medicaid spending per person tend to have lower or no copays.
Can a pharmacist switch my brand-name drug to a generic without my doctor’s permission?
In 41 states, yes-if the generic is therapeutically equivalent and the prescription doesn’t say "dispense as written." But some states require the pharmacist to notify the prescriber, and others allow substitution only if the generic is cheaper. Rules vary by state law.
What’s step therapy, and how does it affect generic drug access?
Step therapy means you must try one or more cheaper drugs before Medicaid will pay for a more expensive one-even if your doctor recommends it. Thirty-two states use step therapy for certain drug classes, like antidepressants or arthritis meds. This can delay treatment and lead to worse health outcomes if the first drug doesn’t work.
Are there any generic drugs that Medicaid won’t cover at all?
Yes. Federal law blocks Medicaid from covering certain drug classes, including fertility drugs, weight-loss medications, erectile dysfunction drugs, and cosmetic drugs-even if they’re generic. States can’t override this rule. Some states also exclude generics that are too expensive or have safety concerns, even if they’re not on the federal exclusion list.
How can I find out what generics are covered in my state?
Visit your state’s Medicaid website and look for the "Preferred Drug List" or "Formulary." Most states publish it online and update it quarterly. You can also call your state’s Medicaid helpline or ask your pharmacist to check the current list. Don’t rely on old information-formularies change often.

Monica Puglia
January 11, 2026 AT 12:24Just had to call my pharmacy because they said my metformin was ‘non-preferred’… I had no idea my state’s formulary changed last week 😣. Took 45 minutes on the phone just to get it approved. Why does this have to be so hard? 🥲
George Bridges
January 13, 2026 AT 05:02I’ve been a caseworker for Medicaid for 12 years. The biggest issue isn’t the rules-it’s the lack of communication. Patients get handed a script and sent to the pharmacy, no context. Then they’re confused when they’re told they owe $8. It’s not their fault. We need better handoffs.
Rebekah Cobbson
January 14, 2026 AT 04:40If you’re on Medicaid and taking generics, please, PLEASE ask your pharmacist if it’s on the preferred list. I used to think my doctor knew everything-but turns out, they get formulary updates via email and forget to tell you. I keep a printed list in my wallet now. It saved me $32 last month. Small wins matter.
gary ysturiz
January 15, 2026 AT 09:04Everyone’s stressed about copays but no one talks about how the system pushes people to skip doses. I know someone who stopped taking her insulin because she couldn’t afford the $4 co-pay. That’s not a choice. That’s a death sentence wrapped in bureaucracy. We need $2 generics everywhere.
laura manning
January 16, 2026 AT 09:51It is, however, a matter of public record that the Federal Upper Limit (FUL) is calculated by the Centers for Medicare & Medicaid Services (CMS), pursuant to 42 CFR § 447.324, and is subject to monthly adjustment based on the Average Manufacturer Price (AMP), as defined in 42 U.S.C. § 1396r-8(k)(1). Furthermore, state-specific formulary decisions are not merely administrative-they are fiscal policy instruments that directly impact health equity. The variance in copay structures across states-ranging from $0 to $8-is not a technical oversight; it is a deliberate reflection of state-level political priorities, which, in turn, reflect systemic underinvestment in low-income populations. Therefore, the notion that this is merely ‘confusing’ is a dangerous minimization of structural injustice.
Sumit Sharma
January 17, 2026 AT 04:16India’s public health system covers generics at near-zero cost. Why? Because we treat medicine as a right, not a commodity. The U.S. Medicaid system is a broken market experiment. States are negotiating drug prices like they’re haggling at a flea market. Meanwhile, people die because they can’t afford $1.50 pills. This isn’t policy-it’s negligence dressed in bureaucracy.
Jay Powers
January 18, 2026 AT 20:17I get why states do step therapy but honestly? It feels like playing Russian roulette with your health. My aunt had to try five different antidepressants before they gave her the one her doctor picked. She ended up in the hospital. I wish there was a way to just say ‘trust the doctor’
Lawrence Jung
January 18, 2026 AT 23:05They say Medicaid covers generics but they don’t tell you that the pharmacy gets paid so little they’ll just say ‘out of stock’ and make you wait two weeks. This whole system is rigged. The PBMs and big pharmacies are making money off your suffering. You think you’re getting help? You’re just a number in their spreadsheet
Alice Elanora Shepherd
January 19, 2026 AT 09:44As someone who works in UK primary care, I find the U.S. Medicaid system’s fragmentation deeply concerning. In the NHS, generics are universally covered with no co-payments, and substitution is automatic unless contraindicated. The variation across U.S. states is not just administratively inefficient-it is ethically indefensible. Patients should not be penalized for geographic accident.
beth cordell
January 19, 2026 AT 11:30Just got my insulin for $0!! 🙌 I live in Minnesota. If you’re in a state with $8 copays… I’m so sorry. You deserve better. 💙
Darryl Perry
January 21, 2026 AT 04:49Stop complaining. Medicaid is a welfare program. If you can't afford your meds, don't take them.
Alex Fortwengler
January 23, 2026 AT 04:12They're hiding the truth-big pharma owns the states. The FUL? A scam. The rebates? A lie. They want you dependent. They want you confused. They want you to think it's about money. It's not. It's about control. And they're winning. Wake up.
Eileen Reilly
January 24, 2026 AT 03:05so like… i got my gabapentin denied bc it’s not preferred?? but my doc said it was the only thing that worked?? so i just went to walmart and paid $4 out of pocket… wait is that legal?? idk anymore 😭