Understanding Oedema in Sickle Cell Disease: Causes, Symptoms & Treatments
 Oct, 5 2025
Oct, 5 2025
Oedema Risk Assessment for Sickle Cell Disease
About This Tool
This assessment helps identify potential risk factors for oedema development in individuals with sickle cell disease. It evaluates common triggers and symptoms associated with fluid retention.
Your Risk Assessment Results
Quick Summary
- Oedema in sickle cell disease (SCD) is usually triggered by vaso‑occlusion, chronic anemia, or kidney problems.
- Common signs include swelling of the legs, ankles, hands, face, and abdomen.
- Key treatments involve managing the underlying SCD (hydroxyurea, transfusions), using diuretics, compression therapy, and lifestyle tweaks.
- Seek urgent care if swelling is rapid, painful, or accompanied by fever, shortness of breath, or chest pain.
- Regular monitoring of kidney function and blood pressure helps prevent severe oedema.
What is Oedema?
Oedema is a condition where excess fluid collects in the interstitial spaces of the body, leading to visible swelling. While anyone can develop oedema, people with blood disorders like sickle cell disease face additional risk factors that amplify fluid retention.
What is Sickle Cell Disease?
Sickle Cell Disease is a hereditary blood disorder caused by a mutation in the hemoglobin beta‑gene (HbS), which makes red blood cells stiff and sickle‑shaped. The misshapen cells block small vessels, cause chronic anemia, and damage organs over time.
How Oedema Develops in Sickle Cell Disease
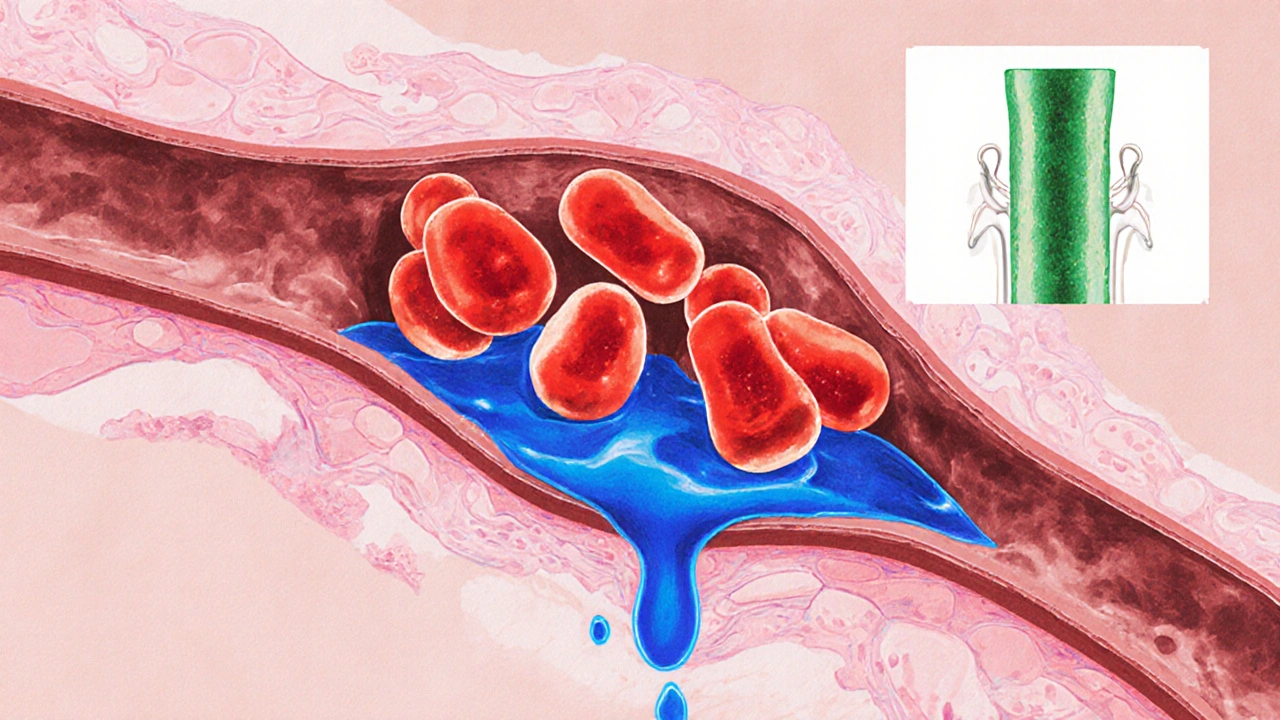
The interaction between Red Blood Cells and the vascular system is at the heart of the problem. Three main pathways generate fluid buildup:
- Vaso‑occlusion: Sickled cells trap in capillaries, raising pressure in the surrounding vessels. The high pressure pushes plasma out of the bloodstream and into surrounding tissue, causing swelling.
- Chronic anemia and low oncotic pressure: Persistent loss of healthy red blood cells lowers plasma proteins such as albumin. With fewer proteins to hold water inside blood vessels, fluid leaks outward.
- Kidney dysfunction: The kidneys filter excess fluid. In SCD, repeated ischemic injury leads to “hyposthenuria” (impaired urine concentrating ability) and eventually chronic kidney disease, reducing fluid excretion.
Additional contributors include heart failure from long‑term high cardiac output and inflammation that makes blood vessels more permeable.
Recognising the Symptoms
Swelling can appear anywhere, but the most typical sites are:
- Lower legs and ankles - often painless, but may feel tight.
- Hands and fingers - especially after a pain crisis.
- Face (periorbital) - common in children during infections.
- Abdomen - can signal ascites, a serious sign of liver or severe kidney disease.
Red flags that demand immediate medical attention:
- Rapidly expanding swelling.
- Painful oedema with a fever (possible infection).
- Shortness of breath, chest pain, or cough (possible pulmonary edema).
- Decreased urine output.
Diagnosing Oedema in SCD
Doctors combine a physical exam with targeted tests:
- Physical assessment: Checking pitting depth, symmetry, and skin temperature.
- Blood work: Hemoglobin level, serum albumin, kidney‑function markers (creatinine, eGFR), and inflammatory markers (CRP).
- Urinalysis: Looking for protein loss, which signals kidney leakage.
- Imaging: Ultrasound of the legs to rule out deep‑vein thrombosis, and chest X‑ray if pulmonary edema is suspected.
Treatment Options
Effective management tackles both the swelling and the underlying sickle‑cell pathology. Below is a snapshot of the most common approaches.
| Therapy | Primary Goal | Typical Dose / Regimen | Key Benefits | Potential Risks |
|---|---|---|---|---|
| Hydroxyurea | Increase fetal hemoglobin (HbF) to reduce sickling | 15‑35mg/kg daily (adjusted by blood counts) | Fewer pain crises, lower risk of vaso‑occlusion‑related oedema | Myelosuppression, skin rash |
| Red Blood Cell Transfusion | Boost oxygen‑carrying capacity, dilute sickled cells | Simple transfusion: 1‑2 units packed RBC; exchange transfusion for severe cases | Rapid reduction of anemia‑driven oedema, improves kidney perfusion | Iron overload, alloimmunisation |
| Diuretics | Promote fluid excretion | Furosemide 20‑80mg PO/IV daily, titrated to urine output | Quick symptom relief, useful for acute swelling | Electrolyte imbalance, dehydration |
| Compression Therapy | Improve venous return | Graduated stockings 20‑30mmHg, worn during daylight | Reduces leg oedema, low side‑effect profile | Skin irritation if too tight |
| Lifestyle & Diet | Support kidney health, control blood pressure | Low‑salt diet (<2g Na/day), adequate hydration (2‑3L water), regular exercise | Long‑term control of fluid balance | None if followed correctly |
Choosing the right mix depends on disease severity, kidney function, and personal tolerance. Many clinicians start with hydroxyurea, add a diuretic when swelling appears, and reserve transfusions for severe or refractory cases.

Practical Home‑Care Tips
- Monitor daily weight: A gain of >2kg over 24hours may signal fluid accumulation.
- Elevate legs when sitting or lying down; use pillows to keep ankles above heart level.
- Wear compression stockings in the morning before getting out of bed; remove if they cause pain.
- Stay hydrated but avoid excess salt: Water helps kidneys flush fluid, while salt traps it.
- Track medication side‑effects: Note any sudden dizziness, muscle cramps, or reduced urine output and report to your care team.
When to Call a Doctor
Even with good home management, certain scenarios require professional care:
- Sudden, painful swelling of the limbs or abdomen.
- Swelling accompanied by fever >38°C (100.4°F).
- Shortness of breath, chest tightness, or coughing up pink frothy sputum.
- Rapid weight gain (>2kg in a day) or a decline in urine volume.
- New‑onset hypertension (BP >140/90mmHg) or worsening blood pressure control.
Emergency departments can provide IV diuretics, imaging, and, if needed, exchange transfusions to reverse the crisis.
Long‑Term Outlook
With modern disease‑modifying therapies, many people with sickle cell disease now live well into their 50s and beyond. Keeping oedema under control is a key piece of that longevity puzzle. Regular follow‑ups with a hematologist, nephrologist, and primary care provider allow early detection of kidney decline, heart strain, and fluid imbalance.
Research in 2024‑2025 is exploring novel agents like voxelotor and gene‑editing approaches that may further reduce vaso‑occlusion, indirectly lowering oedema risk. Staying informed about clinical trials can be empowering for patients seeking the newest options.
Frequently Asked Questions
Why does my leg swell after a pain crisis?
During a crisis, sickled cells block small vessels, raising pressure in the surrounding tissue. The increased pressure forces fluid out of the blood vessels, causing the leg to puff up. Treating the underlying block and using a diuretic can help the swelling subside.
Can I prevent oedema with diet alone?
Diet is a helpful supporting tool but not a cure. Cutting back on salt and staying well‑hydrated reduce fluid retention, yet you’ll still need disease‑modifying therapy (like hydroxyurea) and regular monitoring of kidney function.
Is it safe to take over‑the‑counter diuretics?
Self‑medicating can be risky. Prescription diuretics are dosed based on blood pressure, electrolyte levels, and kidney function. Over‑the‑counter options lack this tailoring and may cause dehydration or low potassium.
How often should I have kidney tests?
Guidelines suggest a full renal panel (creatinine, eGFR, urine protein) at least once a year for stable SCD patients. If you have a history of hypertension or prior kidney issues, your doctor may order tests every 3‑6 months.
Will compression stockings interfere with my daily activities?
Most people find them comfortable once they’re used to the pressure. Choose a size that’s snug but not painful, and wear them during the day; remove them at night to let the skin breathe.

Emma Howard
October 5, 2025 AT 18:10Totally agree that staying on top of kidney labs is key, especially when the swelling starts creeping up. Even a small bump in creatinine can signal you need to tweak diuretics sooner rather than later.
dee gillette
October 5, 2025 AT 19:50While the overview is comprehensive, it neglects to address the socioeconomic barriers that many patients face when accessing regular nephrology care. A more nuanced discussion of insurance limitations would strengthen the piece.
Jasin P.
October 5, 2025 AT 21:14Oh great, another checklist that tells you to “talk to your doctor” – as if they’re not already swamped with paperwork and endless lab results. Maybe the real issue is that the healthcare system is built for paperwork, not patients.
Iain Clarke
October 5, 2025 AT 22:20That’s a fair point. The reality is many clinics lack the dedicated staff to interpret subtle fluid shifts, so a proactive patient approach can make a difference. Regular home weight tracking and blood pressure logs are simple tools that often get overlooked.
Lily Đàn bà
October 5, 2025 AT 23:44Honestly, the drama of swelling after a crisis feels like a plot twist you never asked for. One minute you’re okay, the next your ankles look like balloons at a birthday party.
Conor McCandless
October 6, 2025 AT 00:50Indeed, the cascade of events that follows a vaso‑occlusive episode is nothing short of theatrical – the micro‑thrombi stage, the elevated hydrostatic pressure act, and finally the ominous fluid‑leak curtain call that leaves limbs puffed in a haunting tableau of discomfort; each movement demands a swift inter‑mission of diuretics, compression, and perhaps an urgent exchange transfusion, lest the audience – your body – be forced to endure a prolonged encore of edema that could have been averted with a pre‑emptive hydroxyurea rehearsal.
kat gee
October 6, 2025 AT 02:14Keep moving, stay hydrated, and don’t skip those compression socks – they’re your secret weapon.
Marcia Bailey
October 6, 2025 AT 03:04Exactly! A quick reminder that lifting those socks in the morning before you even get out of bed can prevent a whole day of discomfort. Small habits add up.
Iain Clarke
October 6, 2025 AT 04:10Another thing to keep on your radar is blood pressure – even slight elevations can accelerate fluid retention. If you notice persistent readings above 130/80, bring it up at your next visit.
JOJO Yang
October 6, 2025 AT 05:00I guess that’s it.
Faith Leach
October 6, 2025 AT 06:07Don’t forget the hidden agenda: pharmaceutical companies love to push diuretics without highlighting long‑term electrolyte fallout. Always ask about alternative strategies before you sign up for another pill.
Adam Martin
October 6, 2025 AT 07:47Let’s unpack the whole edema‑SCD interplay because the surface‑level bullet points miss the deeper biology that actually drives the symptoms we see in clinic. First, sickled erythrocytes create micro‑vascular occlusions, which raise capillary hydrostatic pressure; that pressure gradient forces plasma out of the vessels and into the interstitium, initiating the swelling cascade. Second, chronic hemolysis leads to reduced plasma oncotic pressure as albumin levels dip, diminishing the pull that normally keeps fluid inside the vasculature. Third, kidney involvement is a silent but powerful contributor – the hyposthenuria seen in many SCD patients impairs urine concentrating ability, so excess fluid isn’t efficiently excreted. Fourth, repeated vaso‑occlusive crises trigger systemic inflammation, releasing cytokines that increase vascular permeability, essentially opening the floodgates for fluid leakage. Fifth, the heart often works overtime to compensate for anemia, and over time, that high‑output state can strain the myocardium, paving the way for cardiac‑related edema. Sixth, hydroxyurea, while beneficial for reducing crises, can sometimes cause mild renal side effects that need monitoring. Seventh, lifestyle factors such as high dietary sodium exacerbate retention; even modest salt reductions can make a noticeable difference in leg swelling. Eighth, proper use of compression therapy isn’t just about comfort – graded compression improves venous return, reducing the venous pressure that drives fluid out of the capillaries. Ninth, diuretics should be tailored, because over‑diuresis can precipitate acute kidney injury, especially in patients with baseline reduced renal reserve. Tenth, patient education is crucial: teach individuals to track daily weights, monitor for sudden weight gains, and recognize red‑flag symptoms like shortness of breath or chest pain that might signal pulmonary edema. Eleventh, regular labs – BMP, CBC, and urine protein – provide early warnings before clinical edema becomes severe. Twelfth, multidisciplinary care, involving hematology, nephrology, and cardiology, ensures that each organ system’s contribution is addressed. Thirteenth, emerging therapies like voxelotor and gene editing hold promise for reducing sickling and thus downstream edema risk. Fourteenth, participation in clinical trials can give access to cutting‑edge treatments and closer monitoring. Finally, the psychosocial aspect shouldn’t be ignored – chronic swelling affects quality of life, mobility, and mental health, so integrating counseling and support groups can help patients cope while navigating the medical complexities. All these layers together form a comprehensive approach that goes beyond a simple checklist and truly addresses the multifactorial nature of edema in sickle cell disease.
Ryan Torres
October 6, 2025 AT 08:37👍 Great summary! The emoji adds a nice touch, and I love the reminder to keep an eye on weight changes – those subtle shifts can be a game‑changer.
shashi Shekhar
October 6, 2025 AT 09:44Nothing beats the charm of a doctor who thinks “edema” is just “water retention” and forgets the sickle cell context.
Hannah Tran
October 6, 2025 AT 10:34Point taken. If you’re not tracking labs, you’re essentially flying blind. Pressure, proteinuria, eGFR – these aren’t optional data points; they’re the roadmap to catching trouble before it explodes.
Crystle Imrie
October 6, 2025 AT 11:40Edema drama? Too much hype.
Shelby Rock
October 6, 2025 AT 12:30ya man, i think its like when the body tryz to hold onto watr becuz blood cant carry it all, so it ends up in the legz. its a kinda lowkey thing but real.
Dhananjay Sampath
October 6, 2025 AT 13:37Excellent points!; especially the reminder about staying on top of blood pressure;; and using compression wisely.
kunal ember
October 6, 2025 AT 14:27The nuance here lies in the interplay between hemodynamics and renal physiology; when the heart is forced to pump more to compensate for anemia, the resulting increase in central venous pressure can subtly augment peripheral fluid accumulation; meanwhile, the kidneys, already compromised by repeated ischemic insults, may lose their ability to excrete the excess; consequently, a vigilant approach that includes regular echocardiograms to assess cardiac function, alongside periodic 24‑hour urine collections to monitor protein loss, becomes indispensable for preempting clinically significant edema.
Kelly Aparecida Bhering da Silva
October 6, 2025 AT 15:50Don't let anyone tell you that this is just a "minor" issue – swelling can be a warning sign of deeper systemic problems, and ignoring it is practically inviting trouble.