Triptans and SSRIs: The Real Risk of Serotonin Syndrome
 Feb, 12 2026
Feb, 12 2026
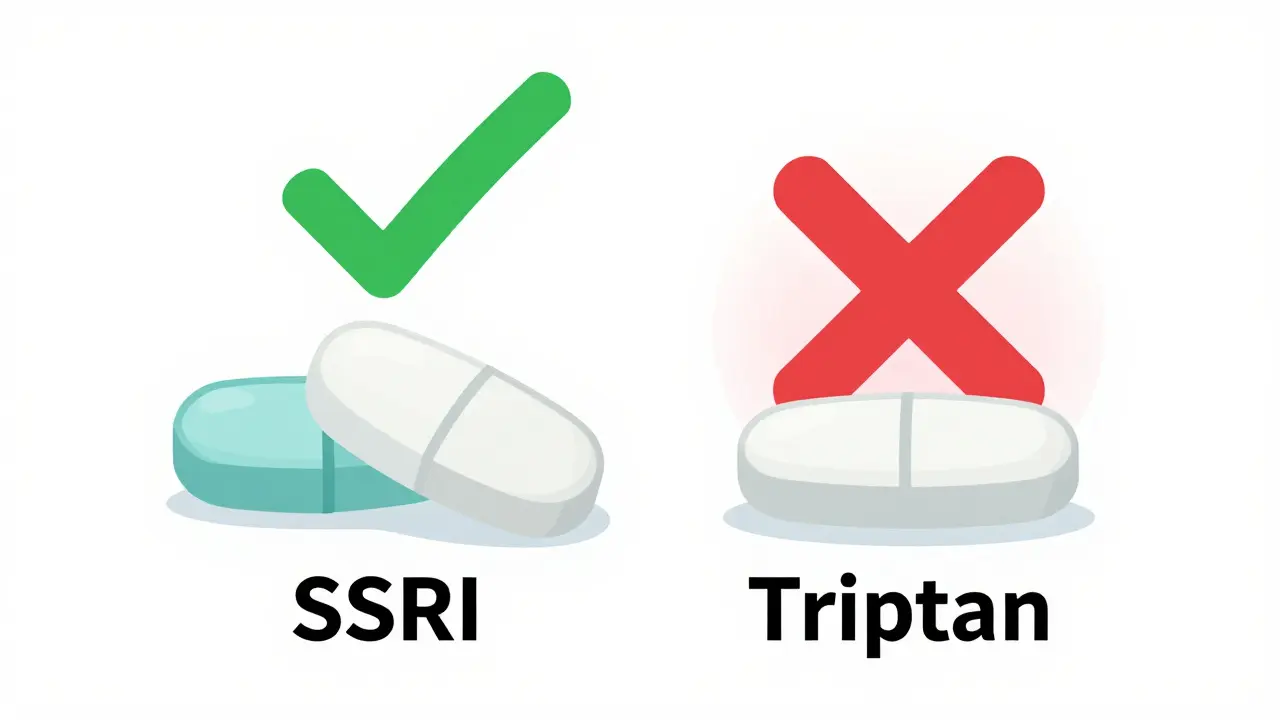
For years, doctors and patients have been told the same thing: if you take an SSRI for depression or anxiety and also get migraines, you can't use triptans. The reason? Serotonin syndrome. It sounded scary-brain fog, muscle rigidity, racing heart, even death. But here's the truth: there is no meaningful risk from combining triptans and SSRIs. Not in practice. Not in real patients. Not even close.
What Even Is Serotonin Syndrome?
Serotonin syndrome isn't just "too much serotonin." That’s a myth. It’s a specific, rare, and dangerous reaction caused by excessive stimulation of certain serotonin receptors in the brain and nervous system. The main culprit? Overactivation of the 5-HT2A receptor. Symptoms show up fast: high fever, shivering, muscle spasms, confusion, fast heartbeat, and sometimes seizures. It’s not something that sneaks up on you. It’s dramatic, unmistakable, and usually happens after a big overdose or mixing two powerful drugs like MAOIs with SSRIs.Now, here’s the twist: triptans don’t work on the 5-HT2A receptor. They target 5-HT1B and 5-HT1D receptors-exactly the ones that calm down overactive blood vessels in the brain during a migraine. They don’t flood your system with more serotonin. They don’t boost overall serotonin levels. They just lock onto a specific target and shut off migraine pain. That’s why, pharmacologically, they shouldn’t even be in the same conversation as drugs that cause serotonin syndrome.
The FDA Warning That Never Made Sense
In 2006, the FDA issued a safety alert. It said: "Don’t mix triptans with SSRIs or SNRIs." Why? Not because anyone had proof. Not because patients were getting sick. But because someone did a theoretical calculation. They looked at the drugs’ mechanisms, saw "serotonin," and assumed danger. No data. No cases. Just guesswork.That warning stuck. Pharmacists started blocking prescriptions. Doctors hesitated. Patients were left with weaker, less effective migraine treatments-like NSAIDs or opioids-just because they were on an antidepressant. And it wasn’t a small group. About half of all migraine sufferers also have depression or anxiety. That’s millions of people told they had to choose between treating their pain or their mental health.
Fast forward to 2019. Researchers at the University of Washington looked at over 61,000 patients who took both triptans and SSRIs over 28 years. Zero cases of serotonin syndrome met diagnostic criteria. Not one. That’s not luck. That’s science. The same study confirmed what pharmacologists already knew: triptans barely touch the receptors linked to serotonin syndrome.
Why the Fear Still Persists
If the evidence is clear, why are so many still afraid?Because warnings stick. Pharmacy software still flashes red alerts when a triptan is prescribed with an SSRI. Some medical charts still carry outdated notes. A 2022 survey found 42% of migraine patients were denied triptans because they were on an antidepressant. And in online forums like Reddit, you’ll find people saying, "My pharmacist refused to fill my prescription. I cried."
It’s not just misinformation. It’s systemic. The FDA warning created a ripple effect. Insurance companies, hospital protocols, even continuing education for doctors-all got caught in the same outdated narrative. Meanwhile, real patients suffered. Migraines got worse. Mental health took a hit. People stopped seeking help because they felt punished for having two common conditions.

What the Experts Really Say
Dr. P. Ken Gillman, a leading migraine researcher, put it bluntly in 2010: "There is neither significant clinical evidence, nor theoretical reason, to entertain speculation about serious serotonin syndrome from triptans and SSRIs."The American Headache Society’s 2022 consensus statement was even clearer: "Clinicians should not avoid prescribing triptans to patients taking SSRIs or SNRIs due to theoretical concerns."
And it’s not just the U.S. The European Medicines Agency never issued a warning. Why? Because they looked at the data-and didn’t see a problem.
Today, 89% of headache specialists routinely prescribe triptans alongside SSRIs. No extra monitoring. No special instructions. Just standard care. And the numbers back it up: triptan prescriptions combined with SSRIs/SNRIs have actually gone up-from 18.7% in 2007 to 32.4% in 2022. Why? Because doctors are finally listening to the evidence, not the alarm.
What You Should Do If You’re on Both
If you’re taking an SSRI or SNRI and need a triptan for migraines, here’s the bottom line:- You can safely take them together.
- You don’t need to taper one or space them out.
- You don’t need to monitor for symptoms unless you’ve had a recent overdose or started a new high-dose antidepressant.
- If your doctor or pharmacist refuses, ask for the latest guidelines from the American Headache Society.
There’s one exception: if you’re on multiple serotonergic drugs-like an SSRI plus an SNRI plus a tramadol or dextromethorphan-then yes, be cautious. But that’s not because of triptans. That’s because of the pile-up of other drugs that *do* raise serotonin levels.

What’s Changing Now?
The tide is turning. In 2023, the American Headache Society and National Headache Foundation formally petitioned the FDA to remove the warning. Their argument? After 17 years, zero confirmed cases. Only 18 unconfirmed reports in the FDA’s own database-none proven to be serotonin syndrome.Meanwhile, the Mayo Clinic updated its patient guidance in 2023: "The theoretical risk has not materialized in clinical practice."
And a major ongoing study tracking 10,000 patients on triptans and SSRIs since 2021 has reported zero cases of serotonin syndrome so far. The data keeps piling up-and it’s not even close to scary.
Why This Matters Beyond Migraines
This isn’t just about triptans. It’s about how medicine works-or doesn’t work. We let theoretical risks dictate real-world care. We let outdated warnings silence progress. We let fear replace evidence.Patients with chronic pain, depression, and anxiety deserve better. They shouldn’t have to choose. And they shouldn’t be told their treatment is dangerous just because two drugs share a chemical pathway. Science has spoken. It’s time for policy, education, and practice to catch up.
Can I take a triptan if I’m on an SSRI for depression?
Yes. Multiple large studies, including one tracking over 61,000 patients over 28 years, found no cases of serotonin syndrome from this combination. Triptans work on different serotonin receptors than those involved in serotonin syndrome. Leading medical organizations now agree the combination is safe.
Why did the FDA warn against it if there’s no real risk?
The 2006 FDA warning was based on theoretical pharmacology, not real-world data. At the time, no large studies had been done. The concern was that both drugs affect serotonin, so they must be dangerous together. But science later showed triptans don’t increase serotonin levels-they just activate specific receptors. The warning was never backed by evidence and has since been contradicted by decades of patient data.
What should I do if my pharmacist refuses to fill my triptan prescription because I’m on an SSRI?
Ask to speak with the pharmacist’s supervisor. Provide them with the 2022 American Headache Society guidelines, which explicitly state that triptans can be safely prescribed with SSRIs/SNRIs. You can also ask your doctor to write a note confirming the combination is medically appropriate. Many pharmacists are still following outdated software alerts and aren’t aware of the latest evidence.
Are there any signs I should watch for if I take both?
If you’re taking only a triptan and an SSRI, you don’t need to monitor for serotonin syndrome. The risk is negligible. But if you’ve recently started a new high-dose antidepressant, added another serotonergic drug (like tramadol, fentanyl, or St. John’s Wort), or taken a large overdose, then seek medical help immediately if you develop symptoms like high fever, muscle rigidity, confusion, or rapid heartbeat. These are signs of a serious reaction-but they’re extremely unlikely to come from just triptans and SSRIs.
Is this still a controversy among doctors?
Among headache specialists, no. Over 89% routinely prescribe triptans with SSRIs without concern. The controversy now exists mostly in outdated guidelines, pharmacy software, and patient myths. The medical consensus has shifted. The real controversy is why it took so long for practice to catch up to the science.

Gloria Ricky
February 13, 2026 AT 02:51Stacie Willhite
February 13, 2026 AT 22:58Jason Pascoe
February 14, 2026 AT 08:17Luke Trouten
February 14, 2026 AT 21:36Brad Ralph
February 15, 2026 AT 19:40Autumn Frankart
February 17, 2026 AT 15:15Skilken Awe
February 18, 2026 AT 16:33andres az
February 19, 2026 AT 11:38