Sugar Intake and Diabetes Medications: How Diet Affects Your Treatment
 Nov, 20 2025
Nov, 20 2025
Sugar Impact Calculator for Diabetes Medication
How Much Sugar Are You Eating?
Track your daily sugar intake and see how it affects your diabetes medication effectiveness.
Add Your Foods
Your Results
Enter your food values to see your medication impact
When you’re taking diabetes medication, what you eat isn’t just about weight or energy-it directly impacts how well your medicine works. Many people think popping a pill is enough to manage their blood sugar. But if you’re drinking sugary sodas, snacking on pastries, or eating fruit juice like water, your meds might as well be on vacation. The truth is simple: sugar intake can make or break your diabetes treatment, no matter what drug you’re on.
Why Sugar Ruins Your Medication’s Effectiveness
Metformin is the most common first-line drug for Type 2 diabetes. It works by telling your liver to stop making too much glucose and helping your muscles use insulin better. But if you eat 100 grams of added sugar a day-about eight teaspoons of sugar in a single soda and a granola bar-your body floods your bloodstream with glucose faster than metformin can handle. Studies show these patients need nearly 30% more metformin just to get the same results as someone eating under 25 grams of added sugar daily. It’s not just metformin. Drugs like glyburide and repaglinide force your pancreas to pump out more insulin. That’s great-if your body has steady carbs to use that insulin. But if you eat a big bowl of pasta or a slice of cake, your blood sugar spikes. Then, a few hours later, when the insulin is still working but the sugar’s gone, your blood sugar crashes. That’s hypoglycemia. People eating inconsistent amounts of sugar on these drugs have up to five times more low-blood-sugar episodes than those who keep carbs steady.What Foods to Avoid (And Why)
Not all sugar is the same. But when you’re on diabetes meds, most added sugars are dangerous. Here are the top seven troublemakers:- Sugary drinks-Soda, sweetened tea, fruit juice. One 12-ounce can of soda has 39 grams of sugar. That’s almost the entire daily limit for someone on a 2,000-calorie diet.
- High-sugar fruits-Mangoes, grapes, cherries. They’re natural, but they pack 20+ grams of sugar per serving. Eat them in small portions with protein or fat to slow absorption.
- Processed snacks-Granola bars, cookies, flavored yogurts. Many have 15-25 grams of hidden sugar per serving. Check labels. If sugar is one of the first three ingredients, skip it.
- White bread and pastries-These are just sugar in disguise. A single slice of white bread can spike blood sugar faster than a candy bar.
- High-fat meals-Fried chicken, creamy pasta, butter-laden toast. Fat slows digestion, which delays sugar absorption. That means your blood sugar doesn’t spike right away-but it stays high for hours, confusing your meds.
- Sweetened alcohol-Margaritas, sangria, cocktails with soda. Alcohol lowers blood sugar, but sugar in drinks raises it. The combo creates wild swings.
- Flavored dairy-Yogurt with “fruit on the bottom,” sweetened milk, protein shakes. These often have 15-20 grams of sugar. Plain yogurt with a few berries is the safe choice.
Even if you’re on newer drugs like semaglutide or dapagliflozin, sugar still matters. These drugs work differently-semaglutide slows digestion and reduces appetite, while dapagliflozin flushes sugar out through urine. But research shows they still lose 15-20% of their power when people eat over 100 grams of added sugar daily. No pill cancels out a junk food diet.
Consistency Is the Secret Weapon
The biggest mistake people make? Eating sugar one day and skipping it the next. Your body needs predictability. If you take glyburide and eat 40 grams of carbs at breakfast one day and 80 the next, you’re setting yourself up for a low-blood-sugar emergency. The Cleveland Clinic’s rule is simple: keep your carb intake within 15 grams of the same amount at each meal. That means if you usually have two slices of whole grain toast and an egg for breakfast, don’t swap it for a bagel and jam without adjusting your meds. This doesn’t mean you can never have dessert. It means plan for it. If you want a small piece of cake at dinner, reduce carbs elsewhere that day. Eat the cake with protein or fat to slow the sugar rush. And always check your blood sugar two hours after eating to see how your body responded.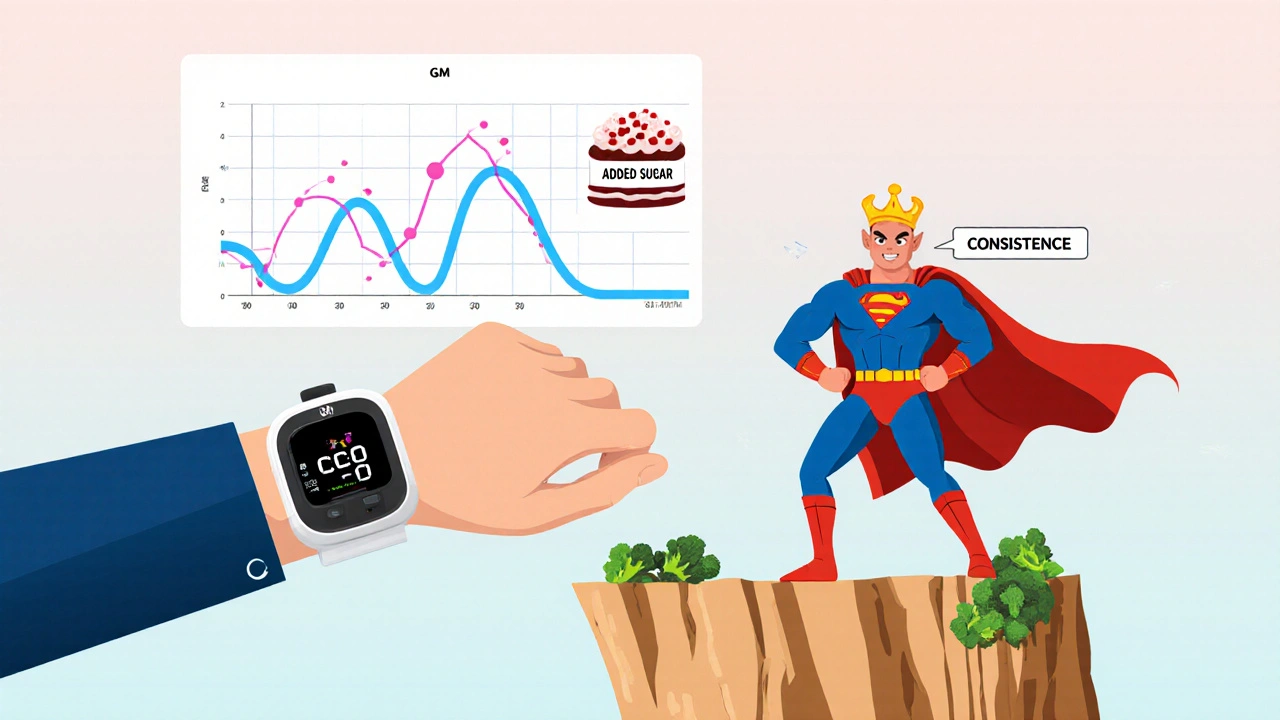
Low-Glycemic Foods Work Better With Your Meds
Not all carbs are created equal. Foods with a low glycemic index (GI)-55 or less-release sugar slowly into your blood. That gives your meds time to work. High-GI foods (70+) dump sugar in fast, overwhelming your system. Good low-GI choices:- Steel-cut oats instead of instant cereal
- Whole grain bread over white
- Legumes like lentils and chickpeas
- Non-starchy vegetables-broccoli, spinach, zucchini
- Apples, pears, berries (in moderation)
Studies show switching to low-GI foods improves insulin sensitivity by 25-40%. That means your metformin works better. Your blood sugar stays lower after meals-often by 35 to 50 mg/dL. That’s the difference between a good day and a hospital visit.
What About Other Medications?
Some drugs you might be taking for other reasons can make sugar control harder:- Prednisolone (a steroid): Can spike blood sugar by 50-100 mg/dL within a day. If you’re on this, you may need temporary insulin or higher metformin doses.
- Furosemide (a water pill): Can interfere with how metformin is cleared by the kidneys. In 32% of cases, this requires a dose adjustment.
- Hormonal birth control: Alters how your body uses glucose. About 27% of women on the pill need their diabetes meds adjusted.
Always tell your doctor everything you’re taking-even over-the-counter supplements. A simple interaction can undo months of progress.
Continuous Glucose Monitors Reveal the Real Story
Many people think their HbA1c test tells the full story. But that’s just an average. A continuous glucose monitor (CGM) shows the spikes and crashes you never see. Data from the DIAMOND study found that people on metformin who ate high-sugar meals had 2.3 times more blood sugar spikes above 180 mg/dL. They spent nearly half their day in high blood sugar-time that adds up to nerve damage, kidney stress, and vision problems. Patients who used CGMs and tracked their food closely saw their HbA1c drop faster. One group using insulin pumps with carb-logging tools had HbA1c levels 0.8% lower than those who guessed their intake. That’s not a small difference-it’s the gap between staying healthy and developing complications.
Why Most People Fail-And How to Succeed
Here’s the hard truth: only 39% of doctors refer newly diagnosed patients to a registered dietitian. That’s a massive gap. You wouldn’t fix a car without a mechanic. Why fix your blood sugar without a nutrition expert? People who get structured nutrition counseling alongside their meds hit their target HbA1c in 6.2 months-almost five months faster than those who just took pills. They also need fewer dose changes and go to the ER 63% less often. The American Diabetes Association says everyone starting diabetes meds should see a dietitian within 30 days. But only 42% of clinics actually do it. Don’t wait for your doctor to suggest it. Ask for a referral. If your clinic won’t help, look for a local diabetes education program or telehealth nutrition service.The Bottom Line
Diabetes meds are powerful tools. But they’re not magic. Sugar intake doesn’t just affect your weight-it directly controls how well your treatment works. You can take the best drug on the market, but if you’re drinking soda with every meal, you’re fighting a losing battle. Start small: swap one sugary drink for water or unsweetened tea. Read labels. Choose low-GI carbs. Keep meals consistent. Track your blood sugar after eating. You don’t need to be perfect. You just need to be consistent.Your body isn’t broken. It’s responding exactly as it should to what you’re feeding it. Change what you eat, and your meds will finally work the way they’re meant to.
Can I still eat fruit if I have diabetes and take metformin?
Yes, but choose wisely. Berries, apples, and pears have less sugar and more fiber than mangoes, grapes, or bananas. Stick to one small serving (about a cup) per meal. Pair it with a handful of nuts or a spoon of Greek yogurt to slow sugar absorption. Avoid fruit juice-it’s sugar in liquid form with no fiber to slow it down.
Does metformin cause weight loss, and can I eat more sugar because of it?
Metformin can help with modest weight loss-usually 5-10 pounds-by reducing appetite and improving insulin sensitivity. But that doesn’t mean you can eat more sugar. High sugar intake cancels out metformin’s benefits and can even cause weight gain over time due to insulin spikes and fat storage. Stick to the limits: under 50 grams of added sugar per day.
Is it safe to drink alcohol while on diabetes medication?
Moderate alcohol can be okay, but avoid sweet cocktails, wine coolers, or mixed drinks with soda. These can spike blood sugar and then crash it hours later. If you drink, choose dry wine, light beer, or spirits with soda water and lime. Never drink on an empty stomach. Check your blood sugar before bed if you’ve had alcohol, because low blood sugar can happen overnight.
Why do I get low blood sugar even when I eat sugar?
This often happens with drugs like glyburide or repaglinide. If you eat a large sugary meal, your body releases a big burst of insulin. When the sugar runs out, the insulin is still working. That’s when your blood sugar drops dangerously low. The fix? Eat consistent, moderate amounts of carbs at every meal. Avoid huge spikes and crashes.
How long does it take to see results from cutting sugar while on metformin?
Most people notice better blood sugar control within two weeks. Fasting levels drop, post-meal spikes shrink, and energy improves. HbA1c may take 3-4 months to show big changes, but daily readings tell the real story. If you cut out sugary drinks and processed snacks, you’ll feel the difference long before your next lab test.
Do I need to count carbs if I’m on metformin?
You don’t need to count every gram, but you do need to be aware. Focus on avoiding added sugars and refined carbs. Choose whole foods. If you eat a meal with 60+ grams of carbs, expect a spike. If you eat 30 grams with protein and fiber, your blood sugar will stay steadier. Use your glucose meter to learn your body’s patterns.
Can I stop my diabetes medication if I eat clean?
Some people do reduce or even stop meds with major lifestyle changes-but only under medical supervision. Never stop your medication on your own. Even if your blood sugar looks normal, your pancreas may still be struggling. Work with your doctor to safely adjust your treatment as your health improves.
What’s the best way to track sugar intake?
Use a free app like MyFitnessPal or Cronometer. They let you scan barcodes and log meals. Focus on tracking added sugars, not total carbs. Aim for under 25-50 grams per day. Write down what you eat and how you feel two hours later. Patterns will emerge quickly. You’ll start noticing which foods make you crash or feel sluggish.

Debanjan Banerjee
November 21, 2025 AT 13:42Just had my HbA1c drop from 8.2 to 6.4 in 4 months after ditching soda and switching to steel-cut oats. Metformin finally started working like it was supposed to. No magic pill-just consistency. If you’re still drinking fruit juice thinking it’s ‘healthy,’ you’re fooling yourself. Fiber matters. Timing matters. Your pancreas isn’t a vending machine.
Steve Harris
November 22, 2025 AT 15:09Really appreciate this breakdown. I’ve been on glyburide for 3 years and had no idea my afternoon granola bar was triggering midnight hypoglycemia. Started tracking with MyFitnessPal and swapped it for almonds and a hard-boiled egg. Blood sugar’s been stable for weeks. Small changes, huge difference.
Michael Marrale
November 23, 2025 AT 00:29Wait… so you’re telling me the pharmaceutical industry doesn’t want you to know that sugar is the real problem? They make billions off meds, but if you just ate right, you wouldn’t need them. Coincidence? I don’t think so. The FDA, ADA, and Big Pharma are all in bed together. They want you dependent. Don’t believe the hype. Eat meat, fat, eggs. Avoid ALL carbs. That’s the real solution.
David vaughan
November 23, 2025 AT 19:50Okay, so… I just read this whole thing. Twice. And I’m crying a little. Not because I’m sad-because I finally get it. I’ve been eating ‘healthy’ granola bars for years. Turns out, they’re just candy with a side of fiber. I switched to plain Greek yogurt with blueberries. My post-lunch crash? Gone. My energy? Better. My metformin dose? Maybe I can ask my doc to lower it. Thank you. Seriously. Thank you.
Cooper Long
November 24, 2025 AT 12:42The data presented is methodologically sound and aligns with current clinical guidelines. The emphasis on glycemic consistency is not merely anecdotal but supported by longitudinal studies published in the Journal of Clinical Endocrinology & Metabolism. The failure of patient education remains a systemic flaw in primary care delivery, particularly in the United States.
Sheldon Bazinga
November 25, 2025 AT 07:00lol so you’re telling me sugar is bad? shocker. next you’ll say breathing oxygen is bad for your lungs. also why is everyone on here acting like they’re some kind of nutrition wizard? I eat what I want, take my meds, and still run marathons. You people need to chill. Diabetes ain’t a diet cult. It’s a medical condition. Stop shaming people.
Sandi Moon
November 26, 2025 AT 22:31How convenient that the ADA, WHO, and every ‘expert’ suddenly agree on sugar’s role-after decades of blaming fat, then cholesterol, then sodium. This is the same playbook used to sell low-fat yogurt with 27g of sugar. The real enemy? Industrialized food systems designed to keep you addicted. They profit from your disease. Don’t be fooled by the glossy infographics. The truth is buried under layers of corporate PR.
Kartik Singhal
November 26, 2025 AT 23:11Bro, I’m from India. We’ve been eating sugar for 5000 years. Ayurveda says sugar is ‘madhura’-sweet, life-giving. Now some American doctor says it’s evil? 🤡 I take metformin, eat jalebi on weekends, and my HbA1c is 6.8. You’re overcomplicating it. Life’s too short to eat boring food. Just check your sugar once a week. Chill.
Logan Romine
November 28, 2025 AT 00:37So… you’re saying the body is a machine that responds predictably to inputs? Wild. Next you’ll tell me gravity exists. I mean, sure, I’ll swap my soda for water… but only because I’m tired of feeling like a zombie after lunch. Also, why do we still call it ‘diabetes’? Sounds like a spaceship from Star Wars. 🤔
Mark Kahn
November 28, 2025 AT 21:17You got this. Seriously. One swap at a time. No need to go full keto or quit fruit forever. Try replacing your morning muffin with an apple and peanut butter. Just one. Then celebrate. You’re not failing-you’re learning. I’ve been there. You’re not alone.
Daisy L
November 29, 2025 AT 14:13Ugh. I just spent 3 hours reading this and now I feel like I’ve been punched in the face by a nutritionist. I drank a smoothie yesterday. A SMOOTHIE. With bananas, honey, and almond milk. And now I’m crying in the cereal aisle wondering if I’m going to lose my toes. Why is this so HARD?!?!?!?!?!
Anne Nylander
November 30, 2025 AT 22:46OMG I JUST REALIZED MY ‘HEALTHY’ YOGURT HAD 22G OF SUGAR!! 😱 I’m swapping it for plain yogurt + strawberries today!! I’m so excited!! My sugar’s been all over the place and I didn’t know why!! Thank you for this!! 💪❤️
Franck Emma
December 2, 2025 AT 05:02I’m done.
Noah Fitzsimmons
December 3, 2025 AT 19:32Wow, so you’re saying the 100+ studies linking sugar to insulin resistance are just ‘coincidence’? And the 30% higher metformin dose needed in high-sugar groups? Just placebo effect? You people are delusional. I’ve seen patients crash from hypoglycemia after eating cake. It’s not ‘diet culture.’ It’s physiology. You’re not special. Your body doesn’t get a pass.
Eliza Oakes
December 4, 2025 AT 04:08Wait-so if I eat sugar and take meds, I’m just ‘fighting a losing battle’? That’s it? No nuance? No ‘it depends on your metabolism, activity level, or gut microbiome’? You’re reducing 10 years of research to ‘don’t eat cake.’ I’m not a robot. I’m a person. And your post feels like a lecture from a teacher who’s never had diabetes.