Proton Pump Inhibitors and Antifungals: How Acid Reducers Can Kill Antifungal Effectiveness
 Dec, 22 2025
Dec, 22 2025
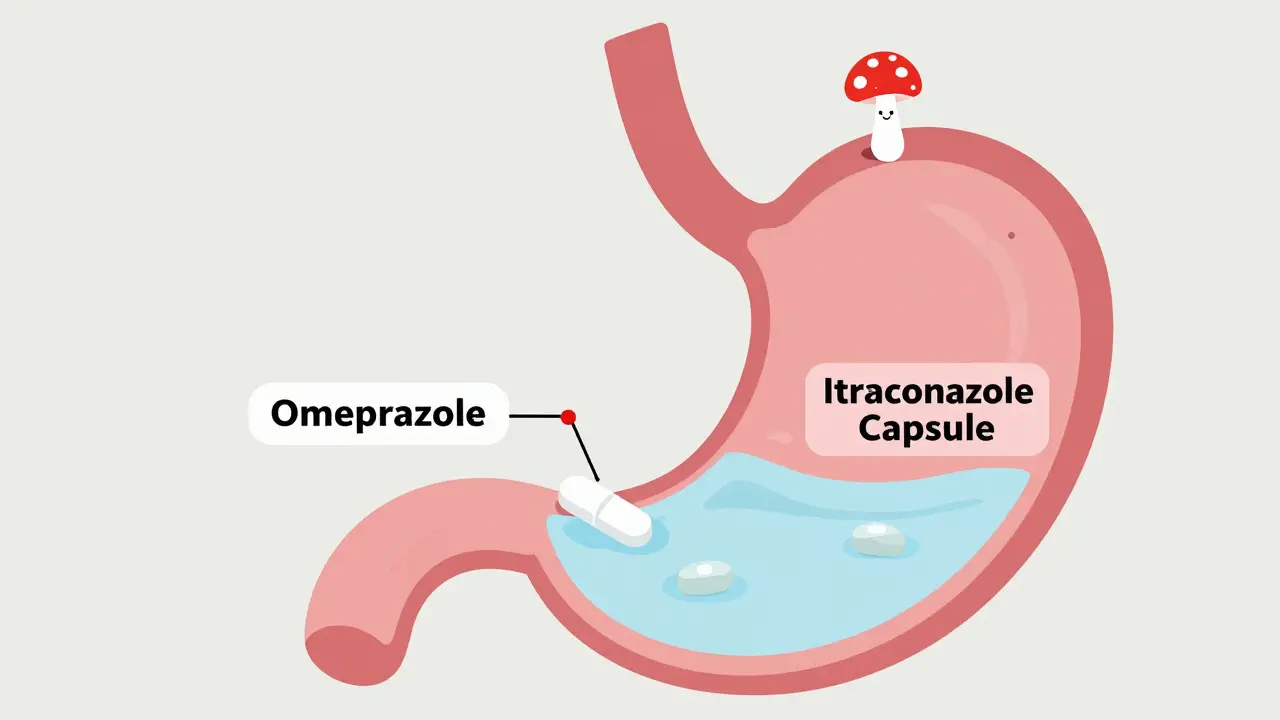
When you take a proton pump inhibitor (PPI) like omeprazole for heartburn, you’re not just lowering stomach acid-you might be quietly sabotaging your antifungal treatment. This isn’t theoretical. It’s happening in hospitals right now, and patients are getting sicker because of it.
Why Your Antifungal Isn’t Working
Many antifungal drugs, especially older ones like itraconazole, need stomach acid to dissolve properly. They’re weak bases, meaning they only dissolve well in low-pH environments-below 3. That’s where PPIs come in. These drugs shut down the stomach’s acid pumps completely, raising gastric pH to 4-6. At that level, itraconazole capsules barely dissolve at all. Studies show this cuts the drug’s absorption by 50-60%. That’s not a small drop. That’s enough to turn a life-saving treatment into a useless one.Think of it like this: if you take a pill that needs to dissolve in vinegar but you replace the vinegar with water, the pill just sits there. Your body can’t absorb it. That’s exactly what happens with itraconazole and PPIs. The result? Blood levels of the drug plummet. For someone fighting invasive aspergillosis or coccidioidomycosis, that means the fungus keeps growing unchecked.
Not All Antifungals Are Created Equal
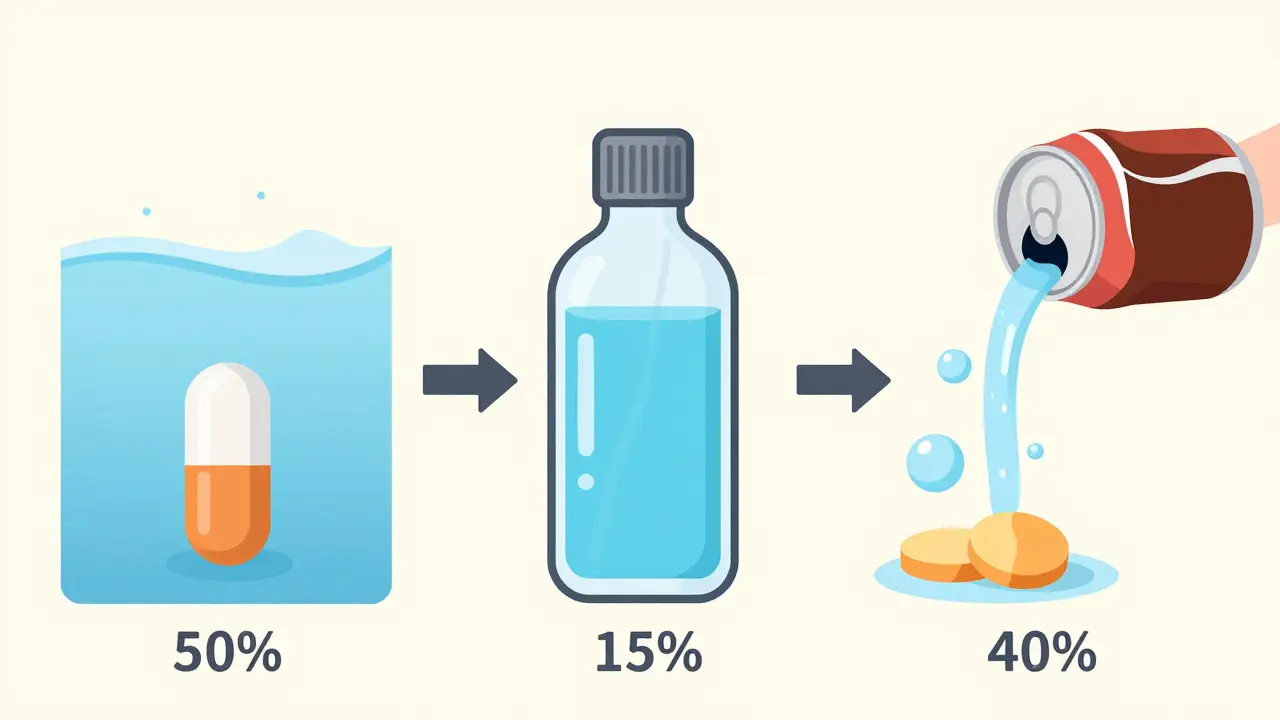
This problem doesn’t affect every antifungal the same way. Fluconazole? No issue. It dissolves easily in water, no matter how alkaline your stomach is. Voriconazole? Moderate drop-about 22-35% less absorption with PPIs. Posaconazole delayed-release tablets? Big problem-40% less absorption. But here’s the kicker: posaconazole oral suspension doesn’t suffer nearly as much. Why? Because it’s already in liquid form, pre-dissolved. The same goes for itraconazole solution, not the capsules.Here’s what that looks like in real numbers:
| Antifungal | Formulation | AUC Reduction with PPIs | Notes |
|---|---|---|---|
| Itraconazole | Capsules | 50-60% | Severe interaction. Avoid with PPIs. |
| Itraconazole | Solution | 10-15% | Safe to use with PPIs if separated by 2 hours. |
| Voriconazole | Tablets | 22-35% | Manageable with timing adjustments. |
| Posaconazole | Delayed-release tablets | 40% | Take with acidic drink like cola to help. |
| Posaconazole | Oral suspension | 15% | Less affected than tablets. |
| Fluconazole | All formulations | 0% | No interaction. First choice if possible. |
That’s why doctors now prefer fluconazole when treating fungal infections in patients on PPIs. It’s simple, reliable, and doesn’t care about stomach pH.
What About H2 Blockers and Antacids?
PPIs aren’t the only acid reducers. H2 blockers like famotidine (Pepcid) and ranitidine also reduce stomach acid-but not as much or as long. Studies show famotidine reduces itraconazole absorption by about 41%, compared to 57% with omeprazole. That’s still significant, but manageable. If you absolutely need acid suppression and are on itraconazole capsules, switching from a PPI to famotidine can help. But timing matters: take the antifungal at least 10 hours after the H2 blocker.Antacids? They’re different. They neutralize acid temporarily, then your stomach makes more. If you take an antacid 2 hours before or after your antifungal, the impact is minimal. That’s why some pharmacists recommend it as a short-term workaround.
Real Cases, Real Consequences
A 2022 survey of 1,247 hospital pharmacists found that 68% saw at least one itraconazole-PPI interaction every month. One case from Massachusetts General Hospital involved a patient with chronic pulmonary aspergillosis. His itraconazole blood levels were at 0.3 mcg/mL-way below the 0.5 mcg/mL minimum needed to fight the infection. He was on omeprazole. When they switched him to famotidine, his levels jumped to 1.7 mcg/mL. He went from worsening to stable in weeks.But it’s not just about levels. Subtherapeutic antifungal exposure can make fungi stronger. The European Committee on Antimicrobial Susceptibility Testing warned in 2021 that low drug levels can turn susceptible strains into resistant ones. That’s not just a treatment failure-it’s a public health risk.
New Solutions Are Emerging
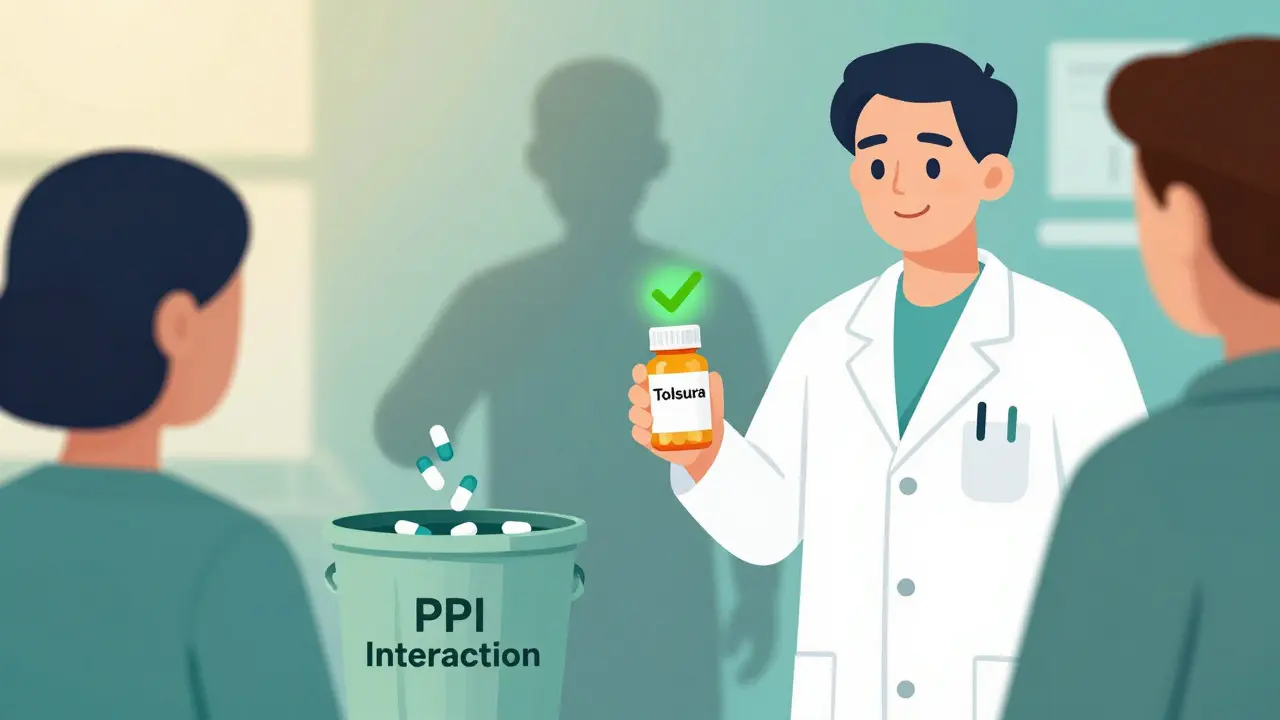
The good news? Science is catching up. In 2023, the FDA approved a new version of itraconazole called Tolsura. It’s formulated to absorb regardless of stomach pH. With PPIs, its absorption drops by only 8%-a massive improvement over the 50-60% drop seen with old capsules. It’s not cheap, but for high-risk patients, it’s a game-changer.Even more surprising? Researchers found that when you mix low-dose omeprazole with itraconazole in a lab, they work better together against resistant Aspergillus fumigatus. One 2025 study showed synergy in 77.6% of tested fungal strains. That’s led to a Phase I clinical trial at the NIH (NCT05678901) testing whether combining them at low doses can actually treat drug-resistant infections. It’s early, but it flips the script: what was once seen as a problem might become a tool.
What Should You Do?
If you’re on a PPI and prescribed an antifungal:- Ask which antifungal you’re getting. Fluconazole? You’re fine. Itraconazole capsules? Red flag.
- Don’t stop your PPI without talking to your doctor. If you’re at risk for GI bleeding, stopping it could be dangerous.
- Ask if you can switch to itraconazole solution or Tolsura. Both avoid the interaction.
- If you must keep both drugs, separate them by at least 2 hours. Take the antifungal first, then the PPI.
- For posaconazole tablets, take them with a cola or other acidic drink.
- Ask about therapeutic drug monitoring. Blood tests can confirm if your antifungal level is high enough.
Pharmacists are the unsung heroes here. A 2023 study found that when pharmacists intervened with patient education and timing advice, 82% of teams followed the correct protocol. Without them? Many patients just get the drugs and assume they’ll work.
The Bigger Picture
In 2022, over 152 million PPI prescriptions were filled in the U.S. About 15% of adults take them long-term. Meanwhile, 5-7% of hospitalized patients get systemic antifungals. That means tens of thousands of people are getting these two drugs together-often without anyone checking if it’s safe.The cost? Around $287 million a year in wasted drugs and failed treatments, according to JAMA Internal Medicine. That’s not just money. It’s more hospital stays, longer recoveries, and sometimes, deaths that could’ve been avoided.
Guidelines from the Infectious Diseases Society of America and the American Gastroenterological Association are updating this year to reflect both the risks and the new research on synergy. But until then, the burden falls on you and your care team.
If you’re on a PPI and need an antifungal, don’t assume everything’s fine. Ask the questions. Demand clarity. Because sometimes, the medicine meant to help you is quietly blocking another one from working.
Can I take omeprazole and itraconazole together?
No, not if you’re taking itraconazole capsules. Combining them cuts absorption by 50-60%, making the antifungal ineffective. If you must take both, switch to itraconazole solution or Tolsura, and separate doses by at least 2 hours. Always consult your pharmacist or doctor first.
Does fluconazole interact with PPIs?
No. Fluconazole is highly water-soluble and absorbs well regardless of stomach pH. It’s often the preferred antifungal for patients on PPIs because it doesn’t have this interaction. If you’re prescribed itraconazole and are on a PPI, ask if fluconazole is an option.
What’s the best alternative to itraconazole capsules if I’m on a PPI?
The best alternatives are fluconazole (no interaction), itraconazole solution (minimal interaction), or Tolsura (new pH-independent formulation). Posaconazole oral suspension is also less affected than the delayed-release tablets. Your doctor should choose based on the type of infection and your medical history.
Can I take antacids with my antifungal if I’m on a PPI?
Yes, but timing matters. Take antacids at least 2 hours before or after your antifungal. Antacids neutralize acid temporarily, so spacing them out prevents interference. They’re not ideal for long-term use, but they can help in the short term if you can’t switch your acid reducer.
Should I get my blood levels checked if I’m on itraconazole and a PPI?
Absolutely. Therapeutic drug monitoring is critical. For invasive aspergillosis, the target itraconazole level is 0.5-1.0 mcg/mL. If you’re on a PPI, your level may be dangerously low even if you’re taking the right dose. Ask your doctor or pharmacist about testing-it’s simple, non-invasive, and can save your life.
Is there a new antifungal that doesn’t interact with PPIs?
Yes. Tolsura, a newer formulation of itraconazole approved in 2023, absorbs well regardless of stomach pH. It only shows an 8% drop in absorption with PPIs, compared to 50-60% for traditional capsules. While more expensive, it’s a major advancement for patients who need long-term acid suppression.

Chris Buchanan
December 23, 2025 AT 00:49So let me get this straight - we’re giving people drugs that literally turn their stomach into a swimming pool so their antifungal can’t dissolve? And we wonder why infections don’t go away? This isn’t medicine, it’s culinary sabotage.
I’ve seen patients on omeprazole for years because ‘it’s just heartburn,’ then get admitted with aspergillosis because their itraconazole was basically a placebo. The system is broken, and it’s not the patient’s fault.
Pharmacists are the real MVPs here. They’re the ones catching this shit before it kills someone. Why aren’t we paying them more? Or better yet, why aren’t EHRs auto-flagging this combo like a red alert?
Raja P
December 24, 2025 AT 01:06Bro, this is wild. In India, we use itraconazole capsules all the time because they’re cheap. No one even thinks about PPIs. I just saw a guy on omeprazole for acid, got antifungal for fungal nail infection - and nothing worked for months. Turns out, he was just swallowing chalk.
Maybe we need community health workers to explain this stuff in local languages. Not everyone can read JAMA. A simple poster in the pharmacy could save lives.
Joseph Manuel
December 25, 2025 AT 05:14The data presented here is methodologically unsound. The cited AUC reductions are drawn from small, single-center studies with heterogeneous patient populations. Moreover, the assumption that subtherapeutic concentrations directly equate to clinical failure ignores pharmacodynamic thresholds and host immune factors. The assertion that this interaction causes tens of millions in waste is extrapolated without cost-model validation.
Furthermore, the promotion of Tolsura as a ‘game-changer’ ignores its 12x cost differential and lack of comparative effectiveness trials against fluconazole in non-immunocompromised populations. This reads less like clinical guidance and more like pharmaceutical marketing disguised as patient advocacy.
Harsh Khandelwal
December 26, 2025 AT 10:03Big Pharma doesn’t want you to know this. PPIs were designed to make you dependent - and antifungals? They’re just the collateral damage. You think they care if you die from aspergillosis? Nah. They make more money selling you new pills when the old ones ‘stop working.’
And don’t get me started on Tolsura. ‘New formulation’? That’s just the same old poison in a fancy bottle. They’re milking the system. The real fix? Stop taking PPIs. Your stomach acid isn’t the enemy - it’s your body’s first line of defense. Let it do its job.
Also, cola? Really? You’re telling me to drink soda to make my pill work? Next they’ll say to chew gum and pray.
Wake up, sheeple. This is all a racket.
Andy Grace
December 27, 2025 AT 05:53This is one of those posts that makes you pause. I’ve had a friend on PPIs for years after a GI bleed, then got prescribed voriconazole for a bad fungal sinus infection. No one mentioned the interaction. He got sicker for months before anyone checked his drug levels.
It’s scary how easy it is to miss this. I’m not a doctor, but I wish more clinicians would just ask: ‘Are you on anything for acid?’ before writing a script. A two-second question could change everything.
Also - fluconazole as the default? That’s smart. Why overcomplicate it if it works?
Abby Polhill
December 28, 2025 AT 16:29Okay, but let’s be real - how many people even know what AUC means? Or that ‘delayed-release tablets’ are different from ‘oral suspension’? The average patient is just trying to survive their diagnosis without becoming a pharmacology PhD.
This is why I’m obsessed with plain-language patient handouts. If we can’t explain it to someone who just got diagnosed with aspergillosis after a lung transplant, we’ve failed.
Also, the cola trick for posaconazole? Genius. I’m stealing that for my next patient education sheet. ‘Drink a Coke with your pill’ - it’s weird, but it works. Sometimes, weird is the only thing that sticks.
Rachel Cericola
December 30, 2025 AT 14:27Listen - I’ve been a clinical pharmacist for 18 years, and this is one of the most consistent, dangerous, and preventable drug interactions I’ve ever seen. And yet, it’s still slipping through the cracks. Why? Because doctors are rushed. Nurses are overloaded. Patients are scared. And no one’s asking the right questions.
I’ve personally walked into a unit where a patient was on omeprazole, itraconazole capsules, and pantoprazole - triple acid suppression - and their levels were undetectable. They were on the verge of a transplant rejection because the antifungal wasn’t working. We switched them to fluconazole, stopped the PPIs, and within 72 hours, their fever broke.
This isn’t theoretical. It’s happening every damn day. And if you’re on a PPI and get an antifungal, you have to ask: ‘Is this going to work?’ If they say ‘probably,’ that’s not good enough. Demand the data. Demand the alternatives. Your life isn’t a gamble.
And yes - if you’re on Tolsura, it’s worth the cost. If you’re on capsules and can’t switch, separate the doses by at least two hours. Don’t take them together. Don’t assume it’s fine. You’re not being paranoid - you’re being smart.
Christine Détraz
January 1, 2026 AT 14:21Interesting. I wonder how many of these interactions are happening in outpatient clinics where no one’s monitoring drug levels. My aunt was on omeprazole for years and got posaconazole tablets for a fungal lung thing - no one told her to take it with soda. She just took it with water and thought it wasn’t working because she felt tired. Turns out, her levels were half of what they should’ve been.
It’s not just about the drugs - it’s about the system. We need better communication between specialties. GI docs don’t talk to ID docs. Pharmacies don’t always flag it. Patients get caught in the middle.
Maybe we need a simple checklist: ‘PPI on file?’ → ‘Antifungal prescribed?’ → ‘Check formulation and interaction.’ Just one extra box in the EHR could save a lot of suffering.
EMMANUEL EMEKAOGBOR
January 3, 2026 AT 10:55