Pharmacodynamic Drug Interactions: How Drugs Amplify or Cancel Each Other’s Effects
 Dec, 28 2025
Dec, 28 2025
When two drugs are taken together, they don’t always just do their own thing. Sometimes, one drug changes how the other works-without changing its level in your blood. This is called a pharmacodynamic drug interaction. It’s not about how your body absorbs, breaks down, or gets rid of the drugs. It’s about what happens at the target site: the receptors, cells, and systems where the drugs actually act. These interactions can be harmless, helpful, or deadly. And they’re far more common than most people realize.
What Exactly Is a Pharmacodynamic Interaction?
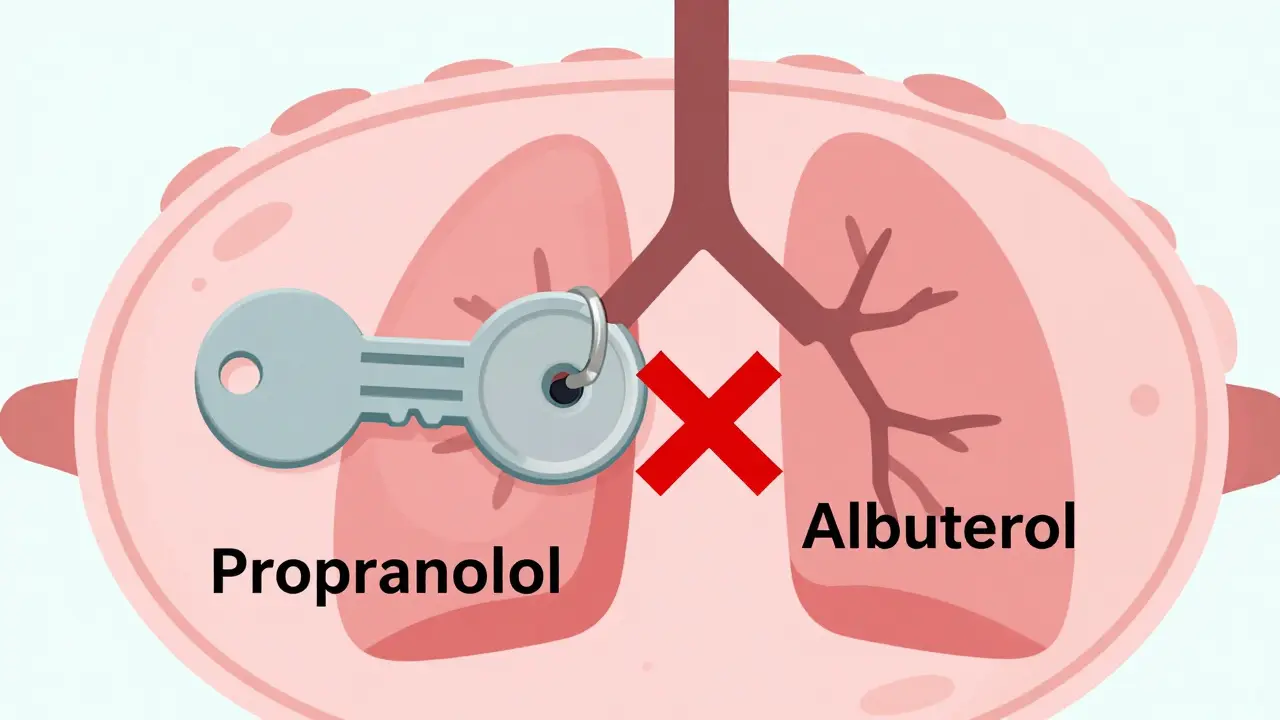
Think of your body’s receptors like locks. Drugs are keys. A pharmacodynamic interaction happens when one key changes how another key fits-or even blocks-the lock entirely. The concentration of either drug might stay perfectly normal, but the result is completely different. That’s why you can’t just rely on blood tests to catch these problems. You need to understand how the drugs behave at their target.
Unlike pharmacokinetic interactions (which involve liver enzymes or kidney clearance), pharmacodynamic interactions don’t change drug levels. They change drug effects. For example, if you take a beta-blocker like propranolol with an asthma inhaler like albuterol, the albuterol might stop working-not because it’s not in your system, but because propranolol is occupying the same receptor sites and blocking it out. This isn’t a mistake in dosing. It’s a clash at the molecular level.
The Three Main Types: Synergy, Additivity, and Antagonism
Pharmacodynamic interactions fall into three clear categories, each with real-world consequences.
- Synergistic: The combined effect is stronger than the sum of the parts. This is how antibiotics like trimethoprim and sulfamethoxazole work together. Each blocks a different step in bacterial folic acid production. Together, they’re far more effective than either alone-reducing the needed dose by up to 75%. This synergy is intentional and life-saving.
- Additive: The total effect is simply the sum of both drugs. Taking acetaminophen and codeine together for pain is additive. Neither drug changes the other’s action; they just stack up. This is often safe, but it’s also where accidental overdose happens. People don’t realize they’re getting two painkillers in one pill.
- Antagonistic: One drug blocks or reduces the effect of another. This is the most dangerous type. NSAIDs like ibuprofen can blunt the blood pressure-lowering effect of ACE inhibitors by cutting kidney blood flow by around 25%. In a 2019 NIH study of 347 hypertensive patients, those taking both had significantly worse control than those on ACE inhibitors alone. For someone relying on that medication to prevent stroke or heart failure, this isn’t just inconvenient-it’s risky.
Receptor-Level Clashes: When Drugs Fight for the Same Target
The most direct form of pharmacodynamic interaction happens at receptors. Drugs compete for the same binding site based on their affinity-how tightly they stick. The drug with higher affinity wins.
Take opioid drugs. Morphine binds tightly to opioid receptors to relieve pain. But if you give naloxone-a drug designed to reverse overdoses-it has even higher affinity. It kicks morphine off the receptor, instantly reversing its effects. In someone dependent on opioids, this doesn’t just stop pain relief. It triggers immediate, severe withdrawal: sweating, vomiting, agitation, even seizures.
Another example: beta-blockers. Propranolol blocks both beta-1 (heart) and beta-2 (lungs) receptors. If someone with asthma takes it, they risk bronchospasm. Even if they’re on a low dose, the drug can shut down the bronchodilating effect of albuterol. That’s why doctors now prefer cardioselective beta-blockers like metoprolol for patients with respiratory issues-they target the heart more than the lungs.
Physiological Interference: When Drugs Disrupt Body Systems
Not all interactions happen at receptors. Sometimes, one drug changes the body’s environment so the other can’t work properly.
NSAIDs like ibuprofen or naproxen reduce inflammation by blocking prostaglandins. But prostaglandins also help keep blood flowing to the kidneys. When you block them while taking an ACE inhibitor or diuretic, your kidneys get less blood. That reduces the drug’s ability to lower blood pressure-and can even cause kidney damage over time. The NHS Specialist Pharmacy Service lists over 280 such interactions as “potentially harmful and contraindicated” based on UK adverse event reports from 2018 to 2022.
Another example: lithium. Used for bipolar disorder, it’s cleared by the kidneys. If you take an NSAID with lithium, your kidneys hold onto more lithium. Levels rise. Toxicity kicks in: tremors, confusion, seizures. This isn’t about liver metabolism. It’s about kidney function being altered by another drug.
The Most Dangerous Combinations
Some pharmacodynamic interactions are so risky they’re considered absolute no-go zones.
- SSRIs + MAOIs: Combining antidepressants like sertraline with MAOIs like phenelzine can cause serotonin syndrome-a life-threatening surge in serotonin. A 2021 meta-analysis found this combination increases serotonin syndrome risk by 24 times. Symptoms: high fever, muscle rigidity, rapid heartbeat, delirium. It can kill within hours.
- Opioids + benzodiazepines: Both depress the central nervous system. Together, they dramatically raise the risk of respiratory failure. The CDC reports this combo was involved in over 30% of opioid-related deaths between 2015 and 2019.
- Anticoagulants + antiplatelets: Warfarin with aspirin or clopidogrel? Double the bleeding risk. A 2022 survey of 1,247 physicians found this was the most common dangerous interaction they encountered monthly.
Even more alarming: 83% of life-threatening pharmacodynamic interactions involve drugs with a narrow therapeutic index-meaning the difference between a helpful dose and a toxic one is tiny. Lithium, digoxin, warfarin, and some seizure medications fall into this category. A small shift in effect can be catastrophic.
When Interactions Help: The Power of Intentional Synergy
Not all pharmacodynamic interactions are bad. Medicine often uses them on purpose.
The combination of naltrexone and low-dose antidepressants is a growing area of research. Naltrexone, normally used for addiction, blocks certain opioid receptors in the brain. When used at very low doses with antidepressants, it appears to reduce inflammation in the nervous system. A 2021 study in the Journal of the American Pharmacists Association showed 68% of patients with treatment-resistant depression improved on this combo-compared to just 42% on antidepressants alone.
Another example: the combination of hydralazine and isosorbide dinitrate in heart failure. Hydralazine relaxes arteries; isosorbide releases nitric oxide to widen them. Together, they improve survival in Black patients with heart failure more than any single drug. This isn’t luck. It’s targeted pharmacodynamics.

Why Clinicians Struggle to Spot Them
Most electronic prescribing systems flag pharmacokinetic interactions-like “avoid this statin with grapefruit juice.” But they’re terrible at catching pharmacodynamic ones. Why? Because they rely on drug levels, not receptor effects.
A 2020 study in Drug Safety found clinical decision systems missed 22% of significant pharmacodynamic interactions. They don’t know that ibuprofen reduces ACE inhibitor effectiveness. They don’t understand that beta-blockers can worsen asthma. They see two drugs and say “no known interaction.”
Doctors and pharmacists are overwhelmed. A 2022 survey showed 63% of physicians encounter a dangerous pharmacodynamic interaction at least once a month. One pharmacist on Reddit described a near-fatal case where linezolid (an antibiotic) and sertraline triggered serotonin syndrome in an elderly patient. It took 72 hours in intensive care to stabilize her.
How to Protect Yourself
Here’s what works:
- Know your drugs. If you’re on a blood pressure med, an antidepressant, or an anticoagulant, ask: “Could anything I’m taking make this less effective-or more dangerous?”
- Use trusted resources. The University of Liverpool’s HIV Drug Interactions database is widely used by specialists. For broader use, Stockley’s Drug Interactions and the NHS Specialist Pharmacy Service database are gold standards.
- Ask for a medication review. A 2021 review in BMJ Quality & Safety found pharmacist-led reviews cut adverse events from pharmacodynamic interactions by 58% in older adults. Most preventable events involved NSAIDs and blood pressure drugs.
- Don’t assume OTC is safe. Ibuprofen, naproxen, even some cold medicines with decongestants can interfere with your prescriptions.
The Future: Better Tools, Better Outcomes
Regulators are waking up. Since 2017, the FDA has required pharmacodynamic interaction studies for new CNS drugs. In 2023, they launched a pilot program expanding this to all new CNS medications. The European Medicines Agency now requires these studies in 34% of new drug applications-up from 19% in 2015.
Research is moving fast. Scientists at UCSF built a machine learning model that predicts serotonin syndrome risk with 89% accuracy. The UK’s NHS is piloting real-time alerts in electronic records that flag not just drug levels, but physiological effects-like “this NSAID may reduce your ACE inhibitor’s effect by 25%.”
By 2050, over 1.5 billion people will be over 65. The average person in that group takes nearly five prescriptions. More drugs = more chances for hidden clashes. Understanding pharmacodynamic interactions isn’t just for doctors anymore. It’s essential for anyone managing multiple medications.
Knowing how drugs interact at the receptor level-not just in the bloodstream-can mean the difference between healing and harm. The science is clear. The tools are improving. What’s left is awareness. And action.

Henriette Barrows
December 28, 2025 AT 13:20Wow, this is such a clear breakdown-I’ve been on a beta-blocker and ibuprofen for years and never realized they could cancel each other out. Thanks for explaining it like I’m not a med student. 😊
Jim Rice
December 28, 2025 AT 14:24You’re oversimplifying. Everyone knows NSAIDs mess with BP meds. This post is just regurgitating Pharm 101. What about the real issue-doctors prescribing 7 drugs to 70-year-olds without checking interactions? That’s malpractice, not pharmacodynamics.
Manan Pandya
December 28, 2025 AT 18:31Excellent summary. I work in a rural clinic in India where patients often combine allopathic and Ayurvedic medications. Many don’t realize that ashwagandha can potentiate sedatives, and turmeric can enhance anticoagulants. This kind of awareness needs to reach beyond Western medical circles.
Joe Kwon
December 29, 2025 AT 11:35TL;DR: Drugs don’t just float around-they *fight* for receptors. SSRIs + MAOIs = serotonin storm 🚨. Opioids + benzos = respiratory arrest 💀. And NSAIDs? They’re the silent killers in the med list. We need AI alerts that don’t just check CYP450 but map receptor-level crosstalk. #PharmDynamics #ClinicalSafety
Nicole K.
December 30, 2025 AT 12:37This is why people shouldn’t be allowed to take pills without a license. My cousin died because she took ibuprofen with her blood pressure med. People are dumb. Stop being so casual with medicine.
Fabian Riewe
January 1, 2026 AT 01:58Man, I used to think ‘drug interaction’ meant grapefruit and statins. Didn’t even know my anxiety med could make my asthma inhaler useless. I switched to metoprolol last year after reading this kind of stuff-life’s been way better. Thanks for the deep dive. 🙌
Amy Cannon
January 2, 2026 AT 23:08While I am of the firm conviction that pharmacodynamic interactions represent a critical frontier in clinical pharmacology, I must express my profound concern regarding the systemic failure of EHR systems to adequately account for receptor-level antagonism. The fact that ibuprofen reduces ACE inhibitor efficacy by 25% is not merely a statistical anomaly-it is a clinical emergency waiting to happen, especially in elderly populations with polypharmacy. I have personally witnessed three cases of iatrogenic renal insufficiency due to this very interaction, and I urge all practitioners to implement mandatory pharmacist-led reconciliation protocols.
Himanshu Singh
January 4, 2026 AT 22:49Great post! I didn't know that naltrexone low dose can help with depression too. My aunt is on it for alcohol and now she's trying it for her mood-hope it works for her too. 😊
Jasmine Yule
January 5, 2026 AT 02:25Okay but why do we still let pharmacies dispense these combos without a warning? I got my NSAID with my lisinopril last week and the pharmacist didn’t say a word. 🤦♀️ I’m done trusting ‘automatic checks’-I’m printing out this post and handing it to my doctor. 📄❤️
Greg Quinn
January 6, 2026 AT 01:35It’s fascinating how we treat drugs like discrete tools, when really they’re more like voices in a crowded room. One shouts, another whispers, another mutes the whole conversation. Maybe the real problem isn’t the drugs-it’s our assumption that biology is linear. What if the body isn’t a machine with parts, but a symphony? And we’re just bad conductors.