Opioids and Adrenal Insufficiency: A Rare but Life-Threatening Side Effect You Need to Know
 Dec, 24 2025
Dec, 24 2025
Opioid Risk Assessment Calculator
Risk Assessment Tool
This tool helps you understand your risk of opioid-induced adrenal insufficiency (OIAI). Based on the article, risk increases significantly when taking opioids for more than 90 days at doses exceeding 20 MME (morphine milligram equivalents) daily.
Your Risk Assessment
Most people know opioids can cause constipation, drowsiness, or addiction. But few realize they can also shut down your body’s natural stress response - and that could kill you.
What Is Opioid-Induced Adrenal Insufficiency?
Opioid-induced adrenal insufficiency (OIAI) isn’t a myth. It’s a real, documented condition where long-term opioid use quietly disables your adrenal glands’ ability to produce cortisol - the hormone your body needs to handle stress, infection, injury, or even a simple fever.
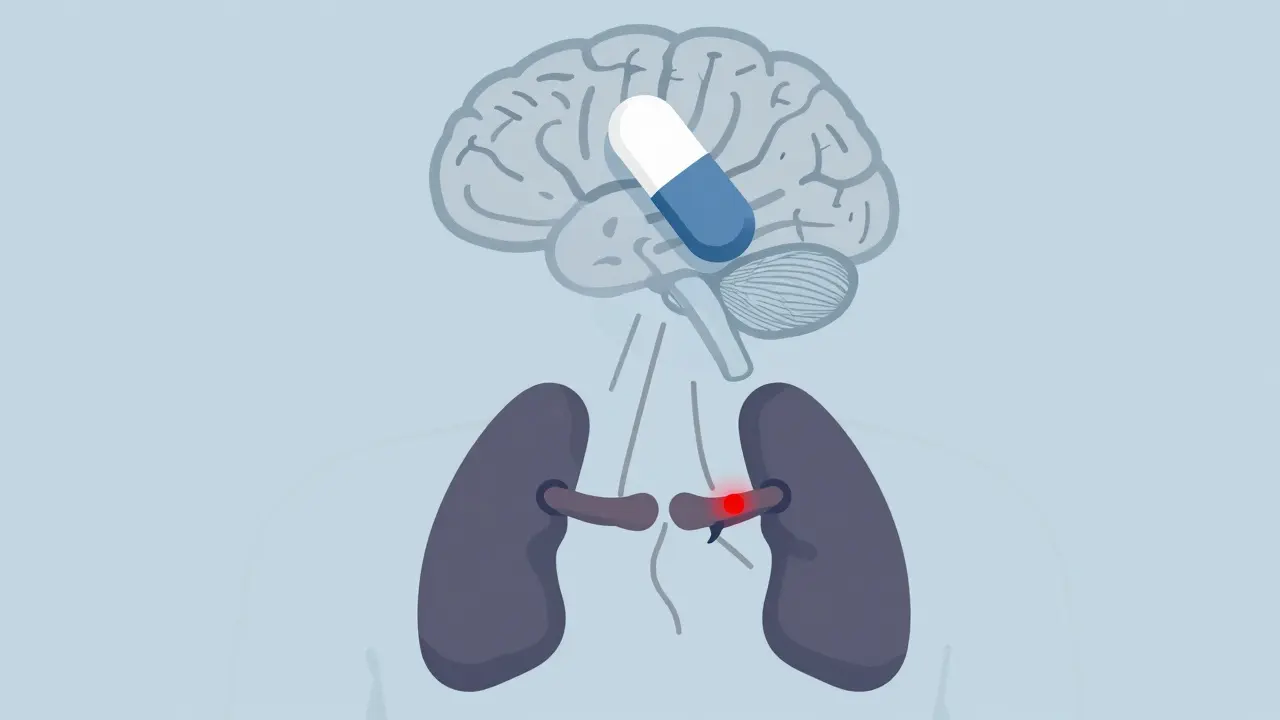
This isn’t damage to the adrenal glands themselves. It’s a communication breakdown. Opioids bind to receptors in your brain’s hypothalamus and pituitary, which normally tell your adrenals: “Release cortisol now.” When opioids block those signals, cortisol production drops. Over time, your body forgets how to make it on its own.
It’s not common - but it’s not rare either. Studies show about 5% of people on chronic opioid therapy develop it. That’s one in every 20 patients. And because symptoms look like fatigue, nausea, or depression - things you might blame on pain or aging - it’s often missed.
Who’s at Risk?
You don’t need to be taking heroin to be at risk. Prescription opioids like oxycodone, hydrocodone, morphine, and methadone can do the same thing.
The biggest red flag? Daily doses above 20 morphine milligram equivalents (MME). That’s roughly:
- 20 mg of oxycodone
- 30 mg of hydrocodone
- 40 mg of morphine
- 15 mg of methadone
A 2020 study found that 22.5% of long-term opioid users failed adrenal stimulation tests - compared to 0% in people not on opioids. The higher the dose and the longer the use, the greater the risk. Some patients on methadone maintenance for years show signs of suppression even at lower doses.
It doesn’t matter if you’re taking opioids for cancer pain, back pain, or after surgery. If you’ve been on them for 90 days or more, your HPA axis is likely affected.
How Do You Know If You Have It?
Symptoms are sneaky. They mimic chronic pain, depression, or just “feeling worn out.” You might feel:
- Constant tiredness, even after sleeping
- Nausea or loss of appetite
- Dizziness when standing up
- Low blood pressure
- Unexplained weight loss
- Muscle weakness
But here’s the danger: during any kind of physical stress - an infection, surgery, car accident, or even a bad flu - your body needs a cortisol surge. If your adrenals can’t respond, you can slip into an Addisonian crisis: dangerously low blood pressure, shock, coma, or death.
Diagnosis requires a simple blood test. A morning cortisol level below 3 mcg/dL is a major warning sign. But the real test is the ACTH stimulation test: you get an injection of synthetic ACTH, and your cortisol levels are checked 30 and 60 minutes later. If your cortisol doesn’t rise above 18 mcg/dL, your adrenals aren’t responding.
Some newer research suggests even lower thresholds might be more accurate, but most clinics still use the 18 mcg/dL cutoff.

It’s Reversible - But Only If Caught
The good news? OIAI isn’t permanent. Once you stop or reduce opioids, your HPA axis can recover - sometimes within weeks, sometimes months.
A 2015 case study followed a 25-year-old man who developed severe hypercalcemia after a hospital stay. Doctors found his cortisol was dangerously low. He was on methadone for chronic pain. When his doctors stopped the methadone and gave him hydrocortisone replacement, his calcium levels normalized and his energy returned. Within six months, his adrenal function was back to normal.
That’s the pattern: stop the opioid, replace cortisol temporarily, and let your body relearn how to make its own.
But here’s the catch: you can’t just quit opioids cold turkey if you’re also adrenal insufficient. Your body needs cortisol support during withdrawal. Without it, you risk a life-threatening crash. That’s why this condition requires a coordinated plan between your pain doctor and an endocrinologist.
Why Is This So Often Missed?
Because no one’s looking for it.
Doctors are trained to watch for addiction, respiratory depression, or constipation. Adrenal insufficiency? It’s not in most pain management guidelines. Even though studies have been published since the 1990s, most clinicians still don’t screen for it.
And when patients say, “I’m always tired,” the default answer is “It’s the pain” or “You’re depressed.” No one thinks to check cortisol.
What’s worse? Opioids don’t affect aldosterone - the hormone that controls salt and potassium. So electrolyte levels often look normal. That gives a false sense of security. You can have adrenal insufficiency and still have “normal” blood tests - unless you specifically test cortisol.

What Should You Do?
If you’re on chronic opioids - especially above 20 MME daily - and you’ve had unexplained fatigue, dizziness, or nausea for months, ask for a cortisol test.
Don’t wait until you’re in the ER with low blood pressure and vomiting. Get tested before a crisis hits.
Here’s what to say to your doctor:
- “I’ve been on opioids for over 90 days.”
- “I’ve been feeling constantly tired, nauseous, or dizzy.”
- “Could my adrenal glands be affected? Can we check my morning cortisol and do an ACTH stimulation test?”
If your doctor says no, ask for a referral to an endocrinologist. This isn’t a specialist issue - it’s a safety issue.
What About Pain Management?
Stopping opioids isn’t easy. And for many, they’re necessary. But you don’t have to choose between pain control and survival.
Some patients successfully switch to non-opioid pain therapies: physical therapy, nerve blocks, cognitive behavioral therapy, or non-addictive medications like gabapentin or duloxetine.
Others taper slowly under supervision, with cortisol replacement during the transition. Once the body recovers, many find they can manage pain with lower doses - or without opioids at all.
And if you absolutely need opioids? Work with your doctor to monitor cortisol levels annually. If your dose goes up, get tested again.
The Bigger Picture
Over 5% of Americans are on chronic opioid therapy. That’s more than 16 million people. If even 5% of them develop adrenal insufficiency, that’s 800,000 people at risk of an undiagnosed, potentially fatal crisis.
This isn’t about blaming patients or doctors. It’s about awareness. We’ve spent years fighting opioid addiction. Now we need to fight the hidden side effects - the ones that don’t show up on a drug test, but can kill you just the same.
Adrenal insufficiency from opioids is rare - but it’s serious. And it’s preventable.
Can opioid-induced adrenal insufficiency be reversed?
Yes, it can. Once opioids are reduced or stopped, the hypothalamic-pituitary-adrenal (HPA) axis usually recovers over weeks to months. Cortisol production returns as the brain relearns how to signal the adrenal glands. In documented cases, patients who tapered off opioids like methadone or oxycodone saw their cortisol levels return to normal within 3 to 6 months, especially when supported by temporary glucocorticoid replacement during withdrawal.
What are the signs of an adrenal crisis from opioid use?
An adrenal crisis is a medical emergency. Signs include sudden severe weakness, dizziness or fainting due to low blood pressure, vomiting, abdominal pain, confusion, and loss of consciousness. These often happen during physical stress - like an infection, surgery, or injury - when your body needs more cortisol but can’t produce it. If you’re on long-term opioids and experience these symptoms, seek emergency care immediately.
Do all opioids cause adrenal insufficiency?
Not all, but most do. Studies show that mu-opioid receptor agonists - like morphine, oxycodone, hydrocodone, fentanyl, and methadone - are the most likely to suppress the HPA axis. Even tramadol and codeine, which are weaker, have been linked to cases. The risk increases with dose and duration, not necessarily the specific drug. Any opioid taken daily for more than 90 days should raise suspicion.
Is adrenal insufficiency from opioids the same as Addison’s disease?
No. Addison’s disease is primary adrenal insufficiency - the adrenal glands themselves are damaged. Opioid-induced adrenal insufficiency is secondary - the problem is in the brain’s signaling, not the glands. That’s why it’s reversible. Your adrenal glands are still healthy; they’re just not being told to work. Treatment is similar (glucocorticoid replacement), but the cause and long-term outlook are very different.
Should everyone on opioids get tested for adrenal insufficiency?
Not everyone - but anyone on chronic opioid therapy (90+ days) with symptoms like fatigue, nausea, dizziness, or low blood pressure should be tested. The American Medical Association recommends screening for patients taking more than 20 MME daily. Routine screening isn’t yet standard, but given the risks, it’s a reasonable precaution if you’re on long-term opioids - especially if you’ve had unexplained health issues.

Zabihullah Saleh
December 25, 2025 AT 16:48It’s wild how we treat pain like it’s the only thing that matters, but ignore the quiet ways opioids break your body from the inside. I’ve seen people on long-term meds who just… fade. No dramatic overdose, no addiction headlines - just exhaustion, weight loss, and then one day, they don’t wake up. No one connects the dots until it’s too late.
This isn’t just a medical issue. It’s a cultural blind spot. We’ve normalized suffering so much that we’ve stopped seeing the cost.
Linda B.
December 25, 2025 AT 20:20So let me get this straight - Big Pharma didn’t just create an addiction crisis… they created a slow-motion murder weapon disguised as pain relief? And now they’re pretending it’s the patient’s fault for not knowing to ask for a cortisol test? Come on. This is the same playbook as cigarettes in the 50s. They knew. They just didn’t care.
Christopher King
December 27, 2025 AT 03:05YOU THINK THIS IS NEW? This has been happening since the 90s. I know a guy who was on 120mg of oxycodone for 7 years - collapsed during a cold. ER docs thought it was a heart attack. Turned out his cortisol was zero. They didn’t even test for it until his wife screamed at them. He’s fine now but lost two years of his life because NO ONE WAS LOOKING. This isn’t rare - it’s covered up. The system doesn’t want you to know you can die from a pill that’s supposed to help.
And don’t even get me started on how endocrinologists are treated like wizards when they dare mention this. ‘Oh you mean the thing that’s in the 2007 JAMA paper? We don’t test for that.’
It’s not medicine. It’s negligence dressed in white coats.
Justin James
December 27, 2025 AT 07:18Let’s be real here - if you’re on opioids for more than 90 days, you’re already gambling with your life on multiple levels, and this adrenal thing is just one more card in the deck you didn’t know was loaded. I’ve read every study on this, and the data is terrifyingly consistent: dose and duration are the only two variables that matter, and doctors are either too busy, too lazy, or too afraid to bring it up because they don’t want to admit they’ve been part of the problem. The fact that we’re still not screening routinely is a moral failure, not a medical one. And the worst part? The people who need this info the most - chronic pain patients who’ve been told to ‘just tough it out’ - are the least likely to ever see it because they don’t have access to specialists or the time to fight for basic tests. This isn’t a rare side effect. It’s a systemic betrayal.
Sophie Stallkind
December 28, 2025 AT 11:02Thank you for this comprehensive and clinically grounded overview. The distinction between primary and secondary adrenal insufficiency is critical, and the emphasis on early screening in high-risk populations is both prudent and overdue. I would encourage clinicians to integrate this into routine monitoring protocols for patients on chronic opioid therapy, particularly those exceeding 20 MME. Early detection not only prevents mortality but also facilitates safer tapering strategies and improved long-term outcomes. This should be standard of care, not an afterthought.
Katherine Blumhardt
December 30, 2025 AT 10:28i just got off 6 months of oxy and was so tired all the time i thought it was depression or my back acting up again but now i think maybe it was this?? my doc never mentioned it and i was on 40mg daily and now i feel better but still kinda dizzy sometimes and i dont know if its the withdrawal or if my adrenals are still messed up??
sagar patel
December 31, 2025 AT 03:53Adrenal suppression from opioids is well documented in endocrinology literature since the 1980s. The mechanism is mediated through mu-opioid receptor inhibition of CRH and ACTH release. The reversibility window is typically 3 to 12 months post-discontinuation, depending on duration of exposure. Screening with morning cortisol and ACTH stimulation test remains gold standard. No controversy. Just negligence.
Bailey Adkison
January 1, 2026 AT 17:55So now we’re blaming doctors for not testing for a condition that’s not even in the official guidelines? What’s next? Should they test for alien abductions too? People get tired. People get nauseous. That’s life. You want to live forever? Stop taking painkillers. Simple. This is just another way to scare people away from opioids so we can all suffer in silence like good little citizens. I’ve been on 30mg oxycodone for 5 years. I’m fine. My cortisol levels are normal. Don’t push your fear onto me.
Gary Hartung
January 2, 2026 AT 17:09Let’s be honest - this isn’t about medicine. This is about control. The pharmaceutical industry, the medical establishment, the DEA - they all have vested interests in keeping you on opioids, because if you stop, they lose money. If you get tested, they have to admit they’ve been lying. If you recover, they lose their captive market. So they bury this in footnotes. They call it ‘rare.’ They say ‘it’s not common.’ But when 5% of 16 million people are affected? That’s 800,000 people who are being quietly sacrificed so someone else can keep making money. This isn’t negligence. It’s calculated. And the worst part? You’ll never see a headline about it. Because the system doesn’t want you to know.
Oluwatosin Ayodele
January 3, 2026 AT 05:55For those in Nigeria or other developing countries, this is irrelevant. We don’t have access to cortisol tests or endocrinologists. We have paracetamol and prayer. If you’re on opioids long-term where I am, you’re either rich or desperate. Either way, you die quietly. No one tests. No one cares. This article is written for Americans who have the privilege to worry about side effects. Most of us are just glad we got the pills at all.
Jason Jasper
January 4, 2026 AT 01:54I’ve been on 15mg oxycodone for 18 months for a spinal injury. I’ve had low energy for over a year, but I thought it was just the injury dragging me down. I never connected it to the meds. I’m going to ask my doctor for a cortisol test next week. I don’t want to wait until I’m in the ER. Thanks for the clarity - this is exactly the kind of info that needs to be out there.
Mussin Machhour
January 5, 2026 AT 07:58Yo if you’re on opioids and feel like a zombie, get tested. Seriously. I was on 40mg of morphine after surgery and felt like I was dragging a couch uphill every day. Got tested - cortisol was half what it should’ve been. Tapered off, got a short cortisol boost, and now I’ve got my energy back. No miracle drug. Just science. Don’t suffer in silence. Ask for the test. Your future self will thank you.