Medication-Induced Angioedema: Swelling Risks and Airway Emergencies
 Feb, 7 2026
Feb, 7 2026
Angioedema Emergency Assessment Tool
This tool helps you assess whether your symptoms might be medication-induced angioedema and whether you need immediate emergency care. Angioedema can be life-threatening when it affects your airway.
Check Your Symptoms
Check Your Medications
Results will appear here after checking your symptoms.
Swelling in your face, tongue, or throat isn’t just uncomfortable-it can stop you from breathing. When certain medications trigger this kind of swelling, it’s called angioedema, and it’s one of the most dangerous drug reactions out there. Unlike a rash or a mild allergic reaction, angioedema attacks the deep layers of skin and tissue, often without warning. And if it hits your airway, you could be in trouble within minutes.
What Exactly Is Medication-Induced Angioedema?
Angioedema is deep swelling under the skin or mucous membranes. It can show up on your lips, eyelids, hands, feet, or inside your throat. When it’s caused by a medication, it’s not always an allergy. In fact, most cases aren’t allergic at all. The two main types are mast cell-mediated (histaminergic) and bradykinin-mediated. The difference isn’t just academic-it changes everything about how you treat it.
Mast cell-mediated angioedema happens when your immune system overreacts to a drug, releasing histamine. This type is often tied to antibiotics like penicillin, NSAIDs like aspirin or ibuprofen, or even some painkillers. Symptoms come on fast: itching, redness, hives, and swelling. It’s the kind of reaction most people think of when they hear "allergy."
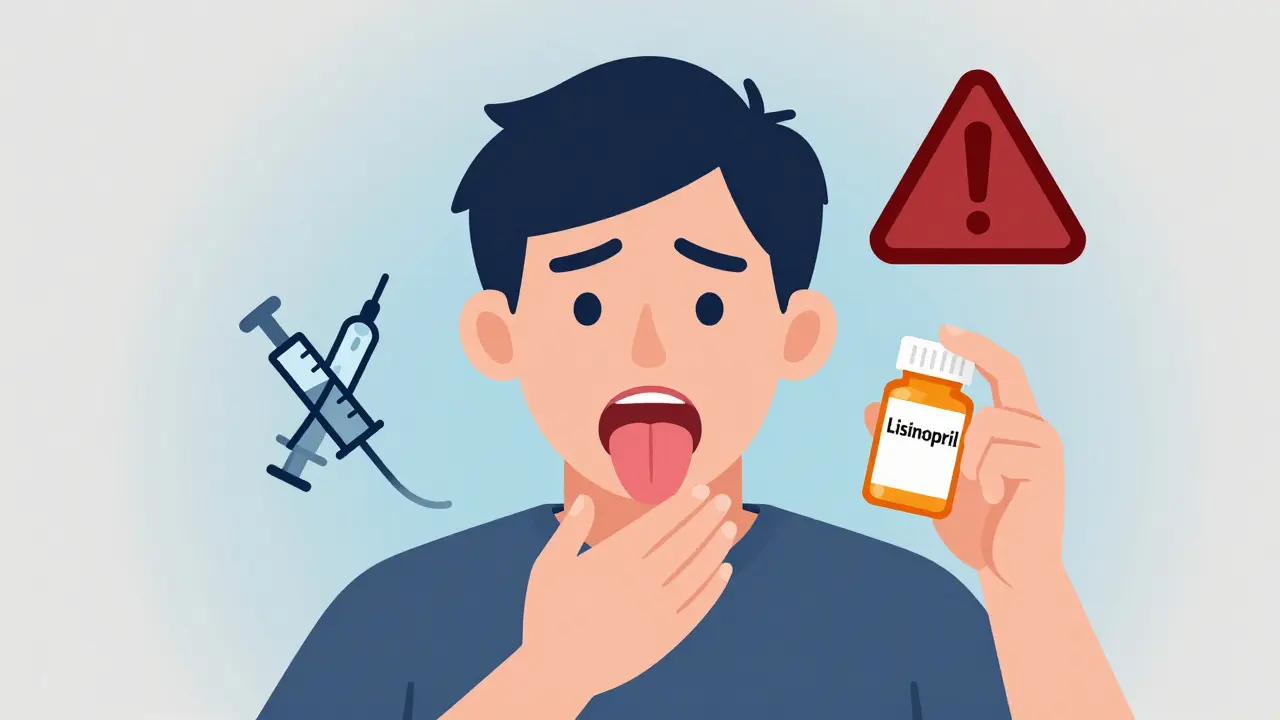
Bradykinin-mediated angioedema is different. It doesn’t involve histamine. Instead, it’s caused by a buildup of bradykinin, a chemical that makes blood vessels leak fluid into surrounding tissue. This is the main culprit behind angioedema from ACE inhibitors-drugs like lisinopril, enalapril, and ramipril. These are commonly prescribed for high blood pressure and heart failure. About 30-40% of all drug-induced angioedema cases come from these medications alone.
Why ACE Inhibitors Are the Biggest Risk
ACE inhibitors have been around since the 1980s. They work well. But they also quietly increase your risk of angioedema. About 0.1% to 0.7% of people taking them will develop swelling. That might sound low, but with over 50 million Americans on these drugs, that adds up to tens of thousands of cases every year. And it’s worse for some groups: African-American patients have up to a 2.2% risk. Women are also more likely to be affected.
The scary part? It can happen anytime-even after years of safe use. Someone might take lisinopril for five years without issue, then wake up one morning with a swollen tongue. Or it might show up after just a week. There’s no reliable way to predict who it will hit. And once it happens, you can’t just "try it again"-the risk of recurrence is about 50% if you restart the same drug.
Even worse, switching to an ARB (angiotensin receptor blocker)-like losartan or valsartan-isn’t a safe workaround. About half of people who had angioedema from an ACE inhibitor will get it again with an ARB. So if you’ve had this reaction before, you need to avoid the whole class of drugs.
Warning Signs: When Swelling Turns Deadly
Not all swelling is an emergency. But when it affects your airway, time becomes your enemy. Here’s what to watch for:
- Sudden swelling of the lips, tongue, or throat
- Changes in your voice-hoarseness or muffled speech
- Stridor-a high-pitched wheezing sound when you breathe
- Difficulty swallowing or feeling like your throat is closing
- Sudden shortness of breath or feeling like you can’t get air in
- Fainting or dizziness
Abdominal swelling can also happen, causing severe pain, nausea, or vomiting. It’s easy to mistake this for food poisoning or appendicitis. But if you’re on an ACE inhibitor and have unexplained belly pain with swelling elsewhere, it could be angioedema.
Studies show that 68% of people with drug-induced angioedema end up in the emergency room because of airway concerns. About 22% need to be intubated to keep their airway open. That’s not rare-it’s common enough that every doctor who prescribes ACE inhibitors should know this risk.
Why Most Treatments Don’t Work
This is where things get dangerous. If you have bradykinin-mediated angioedema from an ACE inhibitor, your standard allergy treatments-epinephrine, antihistamines, and steroids-won’t help. They’re designed for histamine-driven reactions. They do nothing to stop bradykinin.
Yet, this mistake happens all the time. A patient shows up with swollen lips and tongue. The ER gives them Benadryl and prednisone. They send them home. The swelling doesn’t improve. They come back. And again. And again. Some patients report visiting three or more doctors before someone finally connects the dots.
One Reddit user, u/AngioWarrior, shared: "My doctor kept telling me it was just allergies for 3 years while I was on lisinopril-lost 2 teeth from tongue swelling before they finally connected the dots." That’s not an outlier. It’s a pattern.
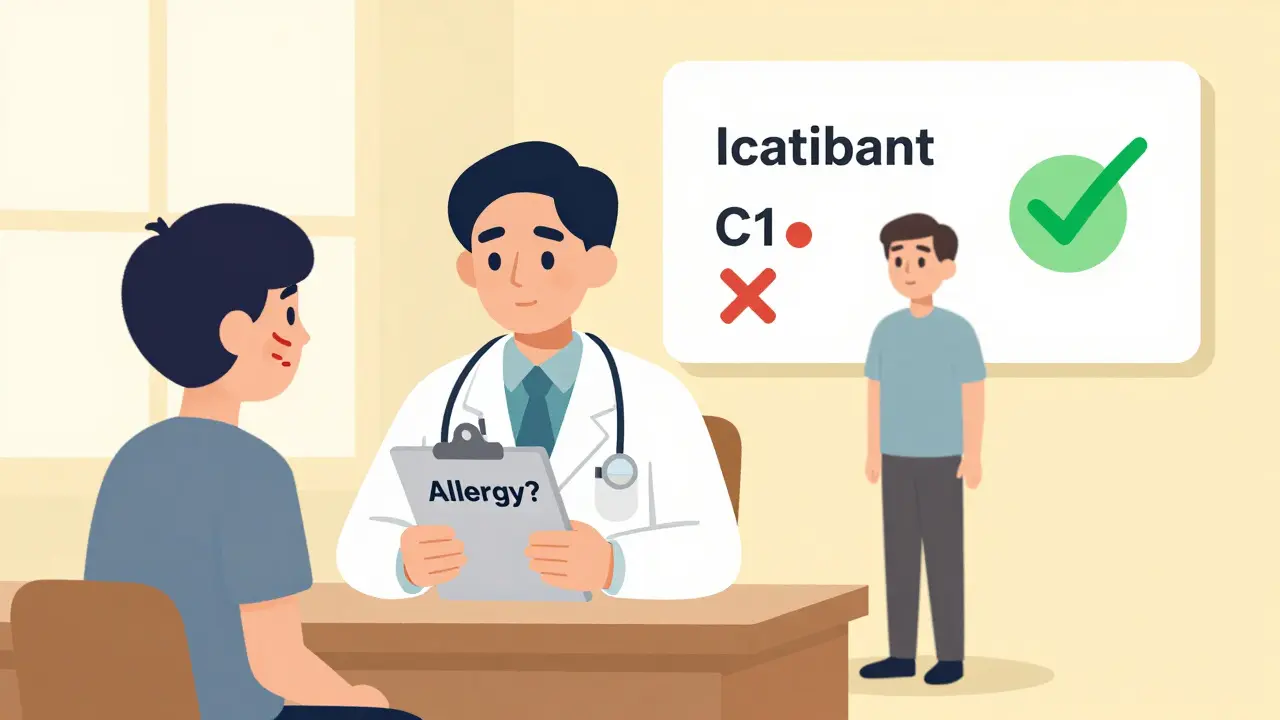
True treatment for bradykinin-mediated angioedema requires specific drugs: C1 inhibitor concentrate, icatibant (a bradykinin blocker), or ecallantide (a kallikrein inhibitor). These are expensive, hard to access, and mostly used in hospitals. For now, the best treatment is stopping the drug, keeping the airway open, and waiting for the swelling to go down-which can take 24 to 72 hours.
What You Need to Do If You’re on These Medications
If you’re taking an ACE inhibitor or ARB, here’s what you should know:
- Know the signs. Swelling in your face or throat isn’t normal. Don’t brush it off as "just allergies."
- Don’t wait. If you notice swelling, especially with breathing trouble, go to the ER immediately. Don’t call your doctor first. Don’t wait until morning.
- Stop the drug. Once you’ve had an episode, you should never take that medication again. Not even a single dose.
- Ask about alternatives. If you need blood pressure control, there are other classes of drugs-calcium channel blockers, diuretics, or beta-blockers-that don’t carry this risk.
- Carry an emergency plan. If you’ve had angioedema before, get a letter from your doctor explaining your condition. Keep it in your wallet. Tell family members what to do if you can’t speak.
For mast cell-mediated angioedema (from penicillin, NSAIDs, etc.), epinephrine auto-injectors (like EpiPen) are life-saving. If you’ve had a reaction like this before, your doctor should prescribe one and teach you how to use it. Carry it everywhere. Use it at the first sign of trouble-then call 911.
The Bigger Problem: Doctors Don’t Know This
A 2022 survey by the American College of Physicians found that only 45% of primary care doctors correctly identified ACE inhibitors as the most common cause of drug-induced angioedema. That’s not a small gap-it’s a crisis.
Most doctors are trained to think of angioedema as an allergy. They treat it with antihistamines. They don’t ask about medications. They don’t consider bradykinin. And patients suffer because of it.
There’s no national protocol for screening. No mandatory warning labels on prescriptions. No routine patient education. The FDA has had a black box warning on ACE inhibitors since 1999-but most patients never see it.
Meanwhile, the global market for angioedema treatments is growing fast-projected to hit $2.4 billion by 2028. But almost all that growth is for rare hereditary forms. The most common cause-medication-induced-is still being ignored.
What’s Changing for the Better
There’s hope. The 2023 International WAO/EAACI guidelines finally gave doctors clear criteria to tell the difference between histaminergic and bradykinin-mediated angioedema. In pilot studies, diagnostic accuracy jumped from 65% to 89%. That’s huge.
New drugs like sebetralstat (approved in 2023) are showing promise for bradykinin-mediated cases-even those caused by medications. These are oral pills, not IV infusions. They’re easier to use. And they could change how we treat this condition in the future.
Experts predict a 30% drop in deaths from medication-induced angioedema by 2028-if doctors start listening. If patients start asking. If we stop treating every swelling as an allergy.
Final Reality Check
Angioedema from medications isn’t rare. It’s not rare for you to get it. It’s not rare for your doctor to miss it. But it is rare for someone to survive a severe airway episode without immediate help.
If you’re on lisinopril, enalapril, or any ACE inhibitor, know your risk. Know the signs. Know what to do. If you’ve ever had swelling after starting a new drug, don’t assume it was "just a reaction." Ask: "Could this have been angioedema?"
Because when your tongue swells shut, no amount of Benadryl will save you. Only recognition. Only action. Only time.
Can you get angioedema from ibuprofen or aspirin?
Yes. NSAIDs like ibuprofen, aspirin, and naproxen can cause mast cell-mediated angioedema, especially in people with a history of asthma or nasal polyps. This type usually comes with hives and itching and responds to antihistamines and steroids. But if swelling happens without hives, it could still be bradykinin-mediated-so don’t assume it’s safe just because you’ve taken it before.
If I had angioedema from lisinopril, can I take losartan instead?
No. About 50% of people who had angioedema from an ACE inhibitor will get it again with an ARB like losartan. The two drug classes work similarly and both can trigger bradykinin buildup. You need to switch to a completely different class of blood pressure medication-like a calcium channel blocker or diuretic.
Does epinephrine work for medication-induced angioedema?
Only if it’s mast cell-mediated (allergic). For angioedema caused by ACE inhibitors or ARBs-which is bradykinin-mediated-epinephrine doesn’t work. It won’t reduce the swelling. Giving it might delay the right treatment. If you’re unsure whether it’s allergic or not, use epinephrine anyway if breathing is at risk-but get to the ER immediately.
How long does drug-induced angioedema last?
Most episodes last 24 to 72 hours. The swelling usually peaks within the first 12 hours. Even if it goes away, you shouldn’t take the drug again. Recurrence is common, and each episode gets harder to manage. In rare cases, especially with hereditary forms, swelling can last up to five days.
Is angioedema from medications hereditary?
No. Medication-induced angioedema is not inherited. But people with hereditary angioedema (HAE)-a rare genetic condition-can have attacks triggered by medications, especially ACE inhibitors. If you have a family history of unexplained swelling, abdominal pain, or throat tightness, talk to an allergist. You may need testing for C1-inhibitor deficiency.

Joseph Charles Colin
February 8, 2026 AT 03:20Medication-induced angioedema is fundamentally a bradykinin dysregulation disorder, not an IgE-mediated hypersensitivity. The clinical distinction is critical: histaminergic reactions respond to antihistamines and corticosteroids, while bradykinin-mediated edema requires targeted inhibitors like icatibant or C1 esterase concentrate. ACE inhibitors inhibit kininase II, leading to unchecked bradykinin accumulation-this is pharmacology 101, yet most ERs still default to Benadryl. It’s a systemic diagnostic failure.
John Sonnenberg
February 9, 2026 AT 09:02This is why we’re losing people. No one takes this seriously until it’s too late. Swelling doesn’t wait for your next appointment. It doesn’t care if you’re ‘just a little congested.’ One minute you’re fine, next minute you’re gasping on the bathroom floor. No jokes. No delays. If your tongue feels thick, go. Now. Not tomorrow. Not after work. NOW.
Tori Thenazi
February 10, 2026 AT 06:21Did you know the FDA knew about this risk since 1999? But they didn’t mandate mandatory patient counseling because Big Pharma lobbied against it. ACE inhibitors are billion-dollar drugs. They don’t want you to know you’re being slowly poisoned by a pill your doctor just scribbled on a prescription pad. And now they’re pushing those new oral drugs-sebetralstat, et cetera-so they can charge $12,000 a month. It’s all profit. No one’s actually trying to save lives. They’re just trying to sell you a new version of the same poison.
Elan Ricarte
February 12, 2026 AT 00:18Let’s be real-the medical system is a carnival of incompetence. You got a guy on lisinopril for five years, wakes up with a swollen tongue, goes to the ER, gets slapped with Benadryl and a pat on the head, sent home. Two days later he’s back, intubated, barely alive. Meanwhile, the docs are like, ‘Huh, weird.’ It’s not weird. It’s predictable. It’s documented. It’s textbook. And yet, we’re still treating this like it’s some mystical mystery illness. We’re not saving people. We’re just waiting for them to die so we can write another sad article about how ‘we didn’t see it coming.’
Scott Conner
February 13, 2026 AT 15:47wait so if i had swelling from ibuprofen is that the same as from lisinopril? i thought it was just allergies
Marie Fontaine
February 14, 2026 AT 09:00Thank you for writing this. 💙 I’ve been on lisinopril for 8 years and never knew this was a risk. I’m scheduling an appointment with my doc this week to switch meds. You saved me. Seriously. ❤️
Ryan Vargas
February 15, 2026 AT 23:50There is a deeper philosophical crisis here: we have outsourced our bodily autonomy to pharmaceutical intermediaries who profit from our ignorance. The fact that a drug class with such a well-documented, life-threatening side effect remains first-line therapy-without mandatory patient education, without standardized screening protocols, without clear labeling on the pill bottle-speaks to a systemic erosion of epistemic responsibility. We are not patients. We are data points in a market-driven algorithm. The angioedema epidemic is not a medical failure. It is a moral one. And until we confront the commodification of health as a foundational societal flaw, no amount of icatibant will fix what’s broken.
Simon Critchley
February 16, 2026 AT 13:04Bradykinin-mediated angioedema is underdiagnosed because it doesn’t fit the allergic paradigm. We’re stuck in a diagnostic rut. The Kallikrein-Kinin system is a nightmare to test for outside academic centers. Most community hospitals don’t have access to bradykinin assays. And even if they did, the clinical presentation overlaps with anaphylaxis, urticaria, even dental abscesses. It’s a diagnostic gray zone-and we treat gray zones with guesswork. That’s why mortality rates remain stubbornly high. We need point-of-care bradykinin biomarkers. Fast. Now.
Jessica Klaar
February 17, 2026 AT 17:22I’m a nurse in an ER in Ohio, and I’ve seen this happen way too many times. A patient comes in, swelling on the tongue, no hives, no itching. We give Benadryl. They get worse. We give steroids. Still worse. Then we finally ask: ‘What meds are you on?’ And it’s always lisinopril. Always. We need a pop-up alert in the EHR. When someone’s prescribed an ACE inhibitor, it should say: ‘WARNING: Risk of angioedema. Educate patient on airway symptoms.’ Simple. But no one’s done it. We’re still flying blind.
glenn mendoza
February 18, 2026 AT 17:01It is with profound gravity that I acknowledge the gravity of this public health concern. The under-recognition of medication-induced angioedema constitutes a grievous lapse in clinical vigilance. I respectfully urge all healthcare providers to institute mandatory patient education protocols at the time of prescription, and to maintain a high index of suspicion for bradykinin-mediated etiologies in the absence of urticaria. Lives depend on our diligence. Thank you for raising this critical issue.
Kathryn Lenn
February 18, 2026 AT 17:06Oh wow. So the same drug that’s supposed to lower my blood pressure is secretly trying to suffocate me? And the FDA’s ‘black box warning’ is just a footnote on page 37 of the 200-page pamphlet I never read? Classic. Next they’ll tell me my antidepressants are just slow-acting poison. I’m switching to yoga and chamomile tea. Or maybe I’ll just stop taking meds altogether. You know, the real solution.
Chima Ifeanyi
February 20, 2026 AT 01:03You Americans are obsessed with drugs. In Nigeria, we use herbs. No angioedema. No side effects. You think your science is better? Look at your hospitals. You’re killing people with pills. ACE inhibitors? That’s colonial medicine. We don’t need your chemicals. We need our roots. Your system is broken. You don’t treat illness-you monetize symptoms.
Monica Warnick
February 21, 2026 AT 23:37I had this happen. Swelling on my tongue. Thought it was allergies. Went to three doctors. One said ‘it’s stress.’ Another said ‘maybe you’re allergic to your dog.’ Finally, a pharmacist asked if I was on blood pressure meds. I was on lisinopril. I cried. I’m so angry. I almost died. And no one told me. No one. Not my doctor. Not my pharmacist. Not even the pill bottle. How is this legal?