How Idiopathic Orthostatic Hypotension Affects Everyday Life
 Sep, 30 2025
Sep, 30 2025
Daily Fluid Intake Calculator for IOH
This tool estimates your recommended daily fluid intake based on your weight and activity level to help manage symptoms of Idiopathic Orthostatic Hypotension (IOH).
When your blood pressure suddenly drops as you stand up, it can feel like the world is tilting. Idiopathic Orthostatic Hypotension is a chronic condition characterized by a significant fall in systolic blood pressure (≥20mmHg) or diastolic pressure (≥10mmHg) within three minutes of standing, without an identifiable underlying cause. People often chalk the dizziness up to “just getting up too fast,” but the reality is far more disruptive.
Quick Takeaways
- Idiopathic Orthostatic Hypotension (IOH) causes sudden drops in blood pressure when standing, leading to dizziness, fatigue, and fainting.
- The condition can limit basic tasks like dressing, cooking, or commuting, and raises the risk of falls.
- Non‑pharmacologic measures-hydration, compression garments, gradual position changes-help many patients.
- When lifestyle tweaks aren’t enough, medicines such as midodrine or fludrocortisone are commonly prescribed.
- Early diagnosis via tilt‑table testing and ongoing monitoring improve quality of life.
What Exactly Is Idiopathic Orthostatic Hypotension?
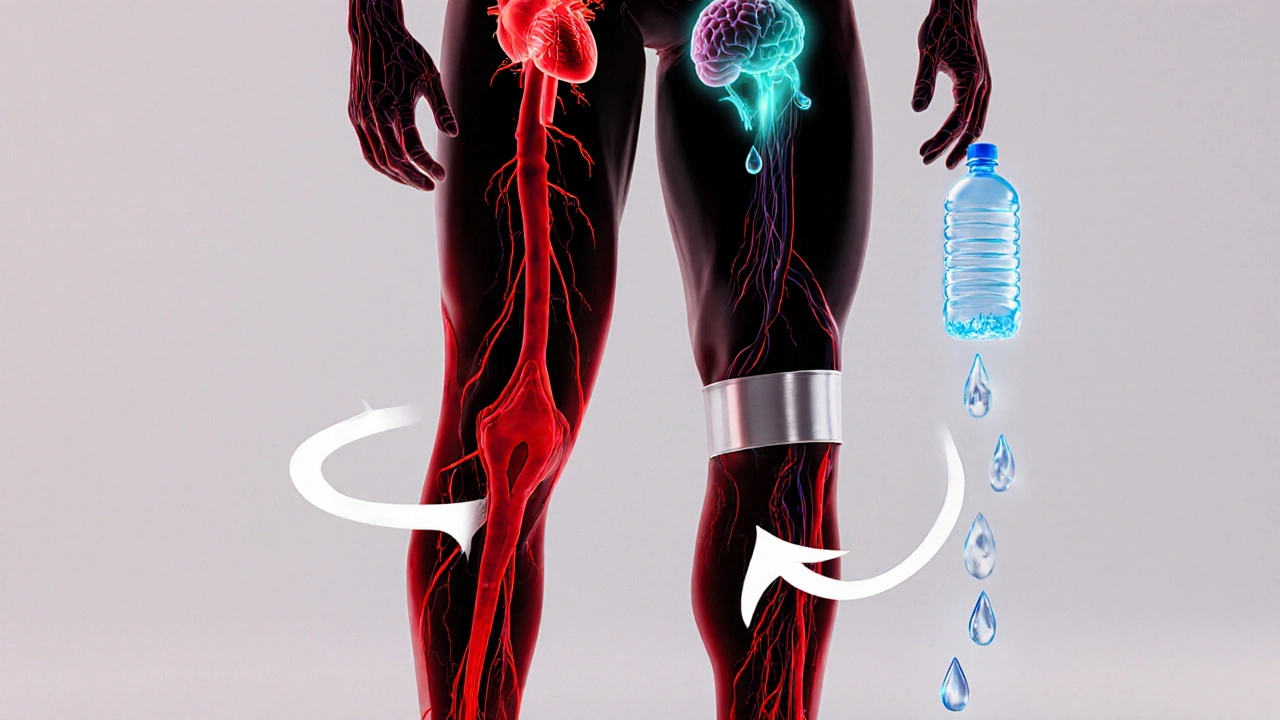
IOH belongs to the broader family of orthostatic hypotension a drop in blood pressure that occurs upon standing and can trigger symptoms like light‑headedness or syncope. What makes the idiopathic form tricky is that doctors cannot pinpoint a secondary cause-no diabetes, Parkinson’s, or medication side‑effect explains the drop. In other words, the body’s autonomic nervous system fails to compensate for gravity‑induced blood pooling.
The autonomic nervous system, or autonomic dysfunction a disorder where the nerves that control involuntary functions such as heart rate and blood vessel tone are impaired, normally constricts veins in the legs and raises heart rate to keep cerebral perfusion stable. When that reflex is blunted, blood pools in the lower extremities, systolic pressure can tumble from 120mmHg to 90mmHg in seconds, and the brain experiences a temporary shortage of oxygen.
How IOH Shows Up in Everyday Activities
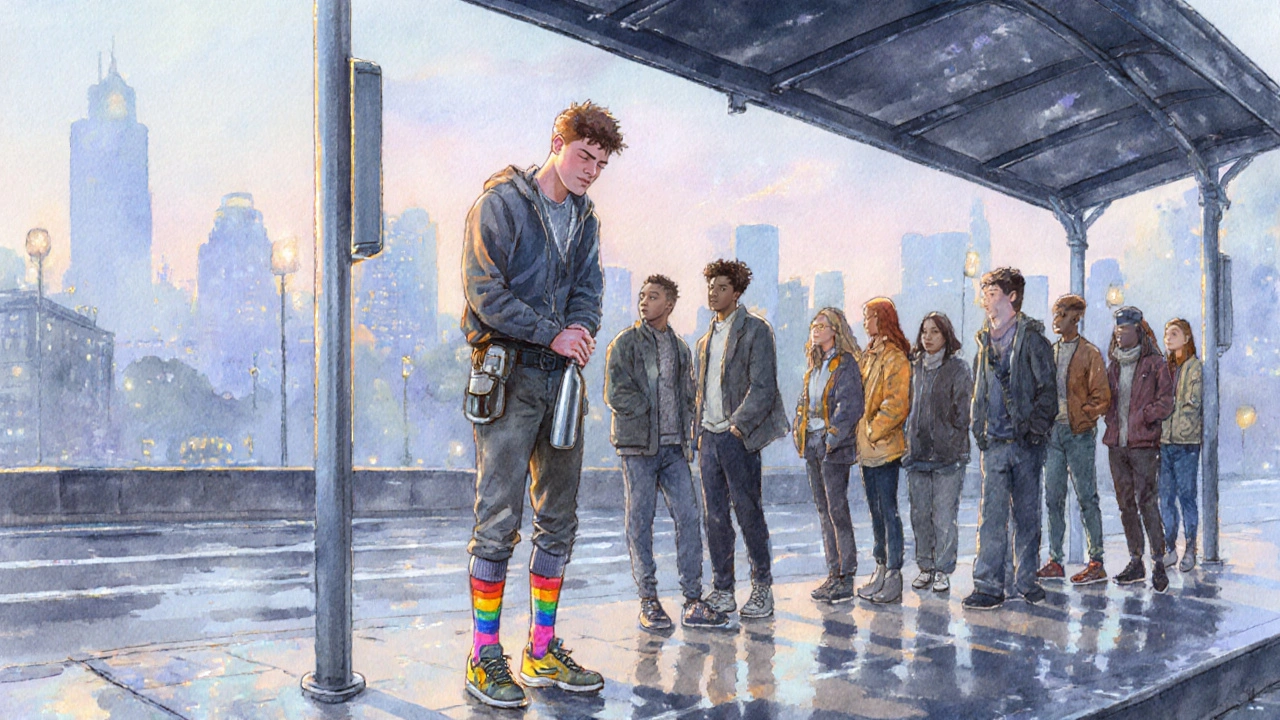
Imagine you’re standing in line at the bus stop on a brisk morning. You feel a sudden wave of light‑headedness, your vision narrows, and within a heartbeat you’re gripping the pole for stability. That’s a classic dizziness a sensation of unsteadiness or spinning that often precedes fainting episode caused by IOH. While a single episode might seem harmless, repeated bouts compound the problem.
Key daily‑life impacts include:
- Morning routine disruption: Getting out of bed can trigger a drop in pressure, making it hard to brush teeth or shower without feeling woozy.
- Workplace limitations: Standing desks, long meetings, or walking to a printer become risky if you haven’t had time to sit and hydrate first.
- Household chores: Bending to pick up laundry, cooking on a stovetop, or lifting groceries can provoke symptoms.
- Social activities: Concerts, crowded pubs, or theme‑park rides involve prolonged standing, often leading to early exit.
- Transportation challenges: Getting on and off buses or trains can cause sudden pressure changes, increasing fall risk.
Each of these scenarios chips away at quality of life the overall perception of wellbeing and ability to engage in desired activities. Surveys of IOH patients report a 30‑40% reduction in self‑reported activity levels, and a two‑fold increase in anxiety about falling.
Risk Zones: Falls, Injuries, and Emotional Strain
Falling isn’t just about bruises; it can lead to fractures, head injuries, or hospital admissions. In people over 65, an orthostatic‑related fall can increase mortality risk by 20%. Even younger adults face lost work days and medical bills.
Beyond the physical, the unpredictable nature of IOH fuels a constant mental checklist: “Do I have water? Did I eat breakfast? Should I sit before I stand?” That mental load contributes to stress, irritability, and sometimes avoidance of activities altogether.
How Doctors Diagnose IOH
The gold‑standard test is the tilt‑table test a controlled examination where a patient is tilted from lying down to an upright position while blood pressure and heart rate are continuously recorded. A positive result shows the required ≥20mmHg systolic drop within three minutes of standing, without other explainable causes. Blood work, medication review, and autonomic function testing round out the assessment.
Because symptoms can overlap with dehydration or medication side‑effects, a thorough review is essential before labeling the condition as idiopathic.
Managing the Condition: Lifestyle First
Most clinicians start with non‑pharmacologic strategies because they’re cheap, safe, and often effective.
- Hydration: Aim for 2-3L of fluid daily. Adding a pinch of salt (if not contraindicated) helps retain water in the bloodstream.
- Compression garments: Knee‑high or waist‑high stockings exert external pressure on veins, reducing pooling.
- Gradual position changes: Sit on the edge of the bed for a minute before standing, and rise slowly from chairs.
- Small, frequent meals: Large meals divert blood to the gut, worsening drops. Eating smaller portions reduces post‑prandial hypotension.
- Elevated head of bed: Tilting the mattress 5-10° keeps blood circulating during sleep.
Tracking blood pressure at home, especially the readings after standing for one and three minutes, helps you see what works and where adjustments are needed.
Medication Options When Lifestyle Isn’t Enough
If symptoms persist, doctors may prescribe drugs that raise vascular tone or increase blood volume.
| Approach | Typical Effectiveness | Onset of Action | Common Side Effects |
|---|---|---|---|
| Compression stockings | Modest (10‑20% BP improvement) | Immediate | Discomfort, skin irritation |
| Midodrine (α‑agonist) | High (20‑30% BP improvement) | 30‑60min | Supine hypertension, scalp tingling |
| Fludrocortisone (mineralocorticoid) | Moderate‑high | 2‑3days | Fluid retention, hypokalemia |
| Increased salt intake | Variable | Hours | Potential hypertension if over‑done |
Doctors weigh the benefits against risks like supine hypertension (high blood pressure while lying down) or electrolyte imbalances. Regular follow‑ups and home BP logs keep the balance in check.
Practical Daily‑Life Tips
- Carry a small water bottle and sip regularly, especially before you know you’ll be standing for a while.
- Wear compression socks every day-put them on before you get out of bed.
- Use a sturdy chair when getting up from the toilet; pause a few seconds before standing.
- Schedule important meetings mid‑morning after you’ve had breakfast and a glass of water.
- If you feel light‑headed, sit or lie down immediately and elevate your legs for a couple of minutes.
- Consider a portable blood pressure cuff; recording a quick standing reading can confirm whether you’re experiencing an IOH episode.
These habits add up; many patients report a noticeable drop in “faint‑time” after a few weeks of consistent practice.
When to Seek Medical Help
If any of the following occur, book an appointment promptly:
- Fainting more than once a month.
- Injury from a fall.
- Persistent dizziness despite hydration and compression.
- New symptoms such as chest pain, palpitations, or shortness of breath.
Early intervention can prevent complications and help you regain confidence in daily tasks.
Frequently Asked Questions
What triggers an idiopathic orthostatic hypotension episode?
The main trigger is gravity pulling blood toward the legs when you stand. If the autonomic nervous system can’t compensate quickly, blood pressure falls and symptoms appear. Dehydration, hot environments, and large meals can intensify the drop.
Can exercise help?
Yes. Gentle resistance training for the lower body improves venous return. Activities like seated leg raises, calf pumps, or short walking intervals can boost the muscles that push blood back to the heart.
Is it safe to take more salt?
For most people with IOH, modest extra salt (up to 1gram extra per day) helps retain fluid and raises blood volume. However, anyone with hypertension or kidney disease should discuss sodium increase with a doctor first.
How long does medication usually take to work?
Midodrine often shows effect within an hour, while fludrocortisone may need a few days to build up. Your doctor will adjust doses based on symptom diaries and home BP readings.
Can I drive safely with IOH?
Driving is generally okay if you’ve taken steps to prevent episodes-stay hydrated, avoid sudden standing, and keep a water bottle handy. If you feel light‑headed while seated, pull over safely and rest before continuing.
Living with Idiopathic Orthostatic Hypotension isn’t about quitting life; it’s about learning the body’s signals and building a toolbox of habits, garments, and, when needed, medicines. With the right strategy, you can keep your mornings steady, your work productive, and your social calendar full.

Liz .
September 30, 2025 AT 20:56Yo, if you’re dealing with IOH just crank up the water and keep a bottle on you at all times. It’s crazy how a simple habit can keep the dizziness at bay.
Stay hydrated and you’ll notice a difference.
luemba leonardo brás kali
October 6, 2025 AT 00:56Managing idiopathic orthostatic hypotension requires a comprehensive approach that includes both lifestyle modifications and careful monitoring of fluid intake. The daily fluid intake calculator you shared is a valuable tool because it tailors recommendations to an individual’s weight and activity level. First, it is essential to understand that hydration status directly influences blood volume, which in turn affects orthostatic tolerance. By ensuring an adequate fluid intake, patients can mitigate the sudden drop in blood pressure that occurs upon standing. Additionally, the calculator prompts users to consider their activity level, which is crucial since more active individuals may lose fluids through sweat more rapidly. It is advisable to spread fluid consumption throughout the day rather than consuming large volumes at once, as this promotes steady absorption. Moreover, incorporating electrolytes, particularly sodium, can help retain water in the circulatory system, though this should be done under medical supervision. Regular monitoring of weight can serve as a proxy for fluid balance; unexpected weight loss may indicate dehydration. Patients should also be aware of the symptoms of overhydration, such as hyponatremia, and seek professional guidance if they experience confusion or severe headache. In practice, using the calculator twice daily-once in the morning and once in the evening-offers a balanced intake that aligns with circadian variations in blood pressure. Keeping a log of fluid intake alongside symptom tracking can provide valuable data for clinicians to adjust treatment plans. It is also recommended to avoid alcohol and caffeine in excess, as they can exacerbate orthostatic symptoms. Finally, while the calculator is an excellent starting point, individualized care plans should be developed in collaboration with a healthcare provider who can consider comorbid conditions and medication effects. Consistent adherence to these guidelines can markedly improve quality of life for those living with IOH.
Corey McGhie
October 11, 2025 AT 04:56Wow, because standing up is apparently the most terrifying thing ever, right? But hey, you’ve actually got a solid plan with that fluid calculator, so kudos for not just rolling over in bed. Just remember to sip water like it’s a trendy Instagram challenge and maybe set a reminder so you don’t forget. It’s not rocket science, but it’s definitely a step up from ignoring the symptoms.
Ajayi samson
October 16, 2025 AT 08:56Honestly, anyone still relying on a spreadsheet to manage a medical condition is just lazy. If you want real results, get off the couch and see a specialist instead of pretending a web form will fix everything. This is basic self‑care, not a miracle cure.
Kathryn Jabek
October 21, 2025 AT 12:56It is incumbent upon individuals afflicted with idiopathic orthostatic hypotension to adopt a regimented hydration protocol, lest they succumb to the debilitating ramifications of insufficient cerebral perfusion. Neglecting such fundamental measures is tantamount to willful self‑sabotage, and one must not permit such negligence to persist.
Ogah John
October 26, 2025 AT 15:56Ah, the lofty rhetoric of disciplined self‑care-how refreshing. One might argue that the cosmos itself conspires to keep us upright, yet we persist in questioning the simplest act of drinking water. Perhaps the true lesson lies in recognizing that even the most profound admonitions reduce to the humble act of staying hydrated.
Kelvin Murigi
October 31, 2025 AT 19:56For anyone looking to implement the calculator effectively, consider pairing it with a daily log that records both fluid volume and any orthostatic symptoms you experience. Over time, you’ll be able to identify patterns-like whether certain activities correlate with increased dizziness-and adjust your intake accordingly. Also, don’t forget to discuss any significant changes with your physician, especially if you’re on medications that affect blood pressure.
ahmad matt
November 5, 2025 AT 23:56So you think a simple calculator is the end‑all, be all? Let me tell you, you probably aren’t even measuring the right variables. You should be tracking heart rate, blood pressure trends, and maybe even doing tilt‑table tests. If you’re not doing that, you’re basically guessing.
Ben Small
November 11, 2025 AT 03:56Drink more water now.
Chidi Anslem
November 16, 2025 AT 07:56While the imperative to increase fluid consumption is sound, it is equally important to calibrate intake to avoid potential hyponatremia, especially in individuals with variable activity levels.
Holly Hayes
November 21, 2025 AT 11:56i cant belive ppl ignore simple advice its just common sense do something for ur health
Penn Shade
November 26, 2025 AT 15:56Actually, the guideline is not just common sense; it is based on physiological principles that dictate plasma volume maintenance through adequate hydration, which you seem to overlook.
Jennifer Banash
December 1, 2025 AT 19:56In the grand theatre of human endurance, the protagonist that neglects the humble act of sipping water becomes a tragic figure, destined to falter upon the very stage of daily life.