Folate Deficiency Explained: Causes, Symptoms & Effective Treatments
 Oct, 6 2025
Oct, 6 2025
Folate Deficiency Risk Assessment
Answer the following questions to assess your risk of folate deficiency. This tool helps identify potential risk factors and suggests next steps.
Your risk assessment will appear here after answering the questions.
Ever wondered why a simple vitamin shortfall can mess with your energy, mood, and even a future pregnancy? Folate deficiency is more than just a lab number; it’s a hidden health snag that shows up in fatigue, pale skin, and sometimes serious birth defects. Below we’ll break down what it is, why it happens, how to spot it, and the best ways to fix it - no medical jargon, just clear steps you can act on.
Quick Takeaways
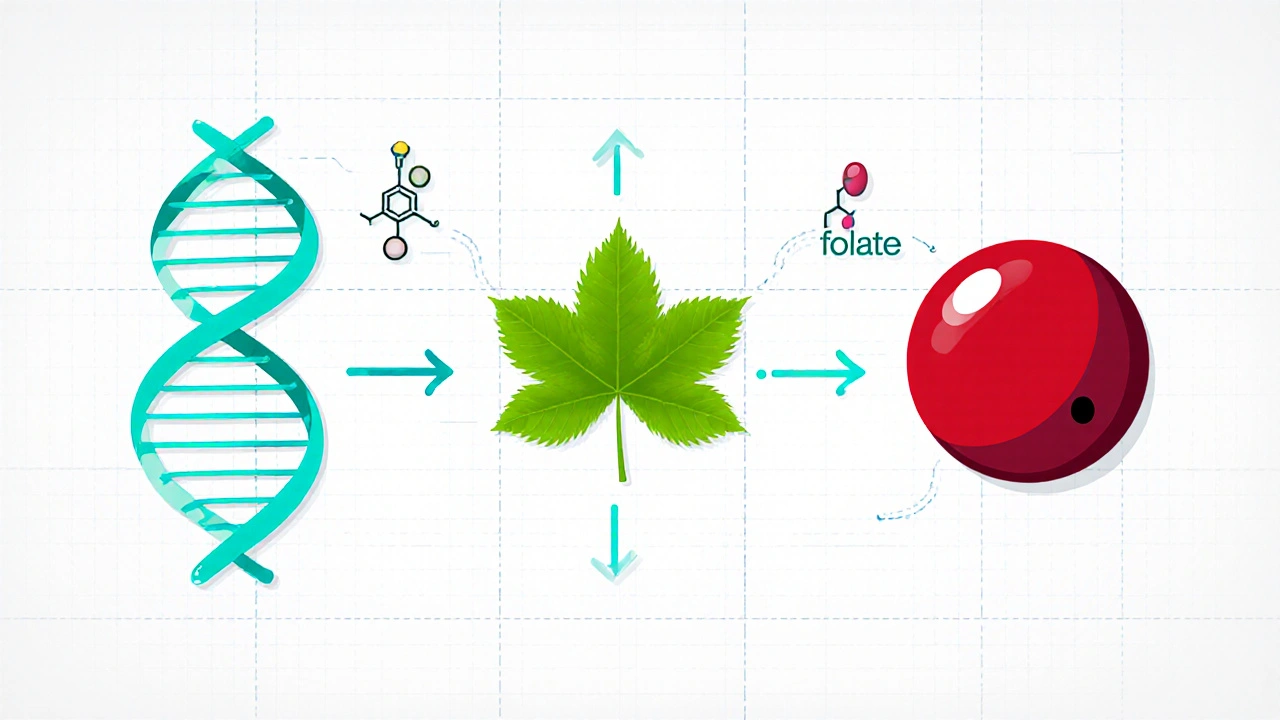
- Folate deficiency occurs when the body lacks enough vitamin B9 to support DNA synthesis and red blood cell formation.
- Major causes include poor diet, alcohol misuse, certain medications, and absorption problems.
- Typical symptoms are fatigue, shortness of breath, glossitis, and, in severe cases, neural tube defects in unborn babies.
- Blood tests measuring serum folate and homocysteine levels confirm the diagnosis.
- Treatment centers on dietary changes, folic acid supplements, and addressing underlying health issues.
What is Folate Deficiency?
Folate deficiency is a condition where the body does not have enough folate (vitamin B9), a water‑soluble vitamin essential for making DNA, RNA, and new cells. Without sufficient folate, the production of healthy red blood cells slows down, leading to a type of anemia.
Key Players in the Folate Story
Understanding the related entities helps you see why the deficiency matters.
- Folate (vitamin B9) is found naturally in leafy greens, legumes, and fortified grains.
- Megaloblastic anemia is the hallmark blood disorder caused by insufficient folate or vitamin B12, characterized by unusually large red blood cells.
- Neural tube defects are birth defects of the brain and spine that can arise when a pregnant woman lacks folate during early gestation.
- Homocysteine is an amino acid that rises when folate (or B12) levels are low, increasing cardiovascular risk.
- Folic acid supplements are synthetic forms of folate used to correct deficiencies quickly.
- Pregnancy amplifies folate needs; a deficit can lead to miscarriage or developmental problems.
Why Does Folate Deficiency Happen? - Common Causes
Pinpointing the root cause guides treatment. Here are the most frequent triggers:
- Poor dietary intake: Diets low in leafy vegetables, beans, and fortified cereals leave you short on folate. Vegans and vegetarians who don’t supplement can be vulnerable.
- Alcohol consumption: Alcohol interferes with folate absorption in the gut and increases urinary excretion.
- Medications: Anticonvulsants (e.g., phenytoin), methotrexate, and sulfasalazine can block folate metabolism.
- Malabsorption syndromes: Conditions like celiac disease, Crohn’s disease, or bariatric surgery reduce the intestine’s ability to absorb folate.
- Increased physiological demand: Pregnancy, rapid growth in teenagers, and hemolytic anemia raise folate requirements.
- Genetic factors: Certain MTHFR gene variants slow the conversion of dietary folate to its active form, folate‑dependent methylfolate.
Spotting the Signs - Typical Symptoms
Folate deficiency often sneaks up on you. Look for these clues:
- Persistent fatigue or weakness despite adequate sleep.
- Shortness of breath during mild activity.
- Pale or yellowish skin (due to anemia).
- Glossitis - a sore, smooth tongue.
- Reduced appetite or unexplained weight loss.
- In severe cases, neurological symptoms (numbness, memory lapses) that overlap with B12 deficiency.
For women of childbearing age, the most concerning outcome is a higher risk of neural tube defects in a fetus.
How Doctors Confirm the Diagnosis
Blood work does the heavy lifting.
- Serum folate test: Measures the amount of folate circulating in the blood. Levels below 3ng/mL typically indicate deficiency.
- Red blood cell (RBC) folate: Provides a longer‑term view of folate stores within cells.
- Homocysteine level: Elevated homocysteine (>15µmol/L) often points to low folate or B12.
- Complete blood count (CBC): Detects megaloblastic anemia - macrocytosis (MCV>100fL) and low hemoglobin.
If the doctor suspects an absorption issue, they may order a short‑term folic acid challenge test to see if supplementation corrects the labs.

Treatment Roadmap - Getting Your Folate Levels Back
Fixing the deficiency usually involves three steps: dietary boost, supplementation, and addressing the underlying cause.
1. Eat Folate‑Rich Foods
Include at least one of these each day:
- Spinach or kale - 1 cup provides about 60µg of folate.
- Black beans - half‑cup gives roughly 130µg.
- Fortified breakfast cereals - often 100‑200µg per serving.
- Avocado - a medium fruit adds 80µg.
2. Supplement Wisely
Standard treatment uses folic acid supplements at 400‑800µg daily for adults. Pregnant women are advised to take 600‑800µg to protect the fetus.
If you have an MTHFR variant, a methylfolate (5‑MTHF) supplement may be more effective because it bypasses the conversion step.
3. Manage Underlying Triggers
- Cut back on alcohol - aim for no more than 1 drink per day for women, 2 for men.
- Discuss medication alternatives with your physician if you’re on anticonvulsants.
- Treat gastrointestinal diseases (e.g., gluten‑free diet for celiac).
- For bariatric patients, lifelong vitamin supplementation is essential.
4. Monitoring Progress
Repeat serum folate and CBC after 6‑8 weeks of therapy. Levels should normalize and anemia markers improve.
Preventing Future Deficiencies
Prevention is easier than cure.
- Make fortified grains a staple - most breads and pastas in the UK are enriched.
- Plan a weekly “green‑leaf” meal (e.g., stir‑fry with broccoli and bok choy).
- Women planning pregnancy should start a prenatal vitamin containing at least 400µg folic acid three months before conception.
- Older adults should have an annual blood check for folate and B12.
Comparison: Folate Deficiency vs. Vitamin B12 Deficiency
| Aspect | Folate Deficiency | Vitamin B12 Deficiency |
|---|---|---|
| Typical anemia type | Megaloblastic anemia (macrocytosis) | Megaloblastic anemia (macrocytosis) |
| Neurological symptoms | Rare, usually mild | Common - numbness, gait problems, memory loss |
| Elevated homocysteine | Yes | Yes |
| Methylmalonic acid (MMA) | Normal | Elevated |
| Primary dietary sources | Leafy greens, legumes, fortified grains | Meat, fish, dairy, eggs |
Frequently Asked Questions
What blood level defines folate deficiency?
A serum folate below 3ng/mL (≈7nmol/L) is considered deficient. RBC folate below 140ng/mL also signals low stores.
Can I fix folate deficiency with food alone?
Mild cases may improve with a diet rich in greens, beans, and fortified cereals. Moderate to severe deficiencies usually need a short course of folic acid supplements (400-800µg daily) for 2-3 months.
Is folate deficiency dangerous during pregnancy?
Yes. Low folate in early pregnancy raises the chance of neural tube defects such as spina bifida. Women planning conception should take at least 400µg of folic acid daily, ideally starting three months before trying to get pregnant.
Do I need to take folic acid if I already eat vegetables?
If you consume several servings of leafy greens and legumes each day, you may meet your needs. However, factors like alcohol, certain meds, or malabsorption can still cause a shortfall, so a low‑dose supplement (400µg) is a safe safety net.
Can folate deficiency cause heart problems?
Elevated homocysteine from low folate is linked to higher cardiovascular risk. Correcting the deficiency can lower homocysteine and may reduce that risk, especially when combined with a heart‑healthy lifestyle.
Bottom line: Folate deficiency is common but easily tackled with the right foods, a dose of supplement, and attention to any medical conditions that block absorption. If you notice the symptoms or fall into a high‑risk group, get a quick blood test and start the simple fix today.

Brenda Hampton
October 6, 2025 AT 12:17Folate deficiency often flies under the radar until you feel constantly drained or notice your skin looking pale. The article does a solid job outlining the key risk factors like poor diet, alcohol use, and certain medications. If you suspect you fall into any of those categories, a quick blood test can confirm the issue. Taking a daily multivitamin with 400 µg of folic acid is a simple first step.
Lara A.
October 12, 2025 AT 00:17-The pharmaceutical oligarchs don’t want you to know that folate supplements are a covert mind‑control tool!-
Ashishkumar Jain
October 17, 2025 AT 12:17Hey folks, great rundown on folate! I’ve always found that adding a handful of spinach to my morning smoothie makes a noticeable difference in energy levels. It’s also cool to see the link between low folate and higher homocysteine, which can affect heart health. If you’re on meds like methotrexate, chatting with your doctor about a folate boost can prevent anemia. And for anyone planning a family, the extra 400 µg a day is like a safety net for your future baby. Keep sharing these practical tips, it helps a lot of us stay healthy.
Gayatri Potdar
October 23, 2025 AT 00:17Listen, the “healthy smoothie” narrative is just a front-big agribusiness wants you to think leafy greens are enough while they pollute the soil. They purposely hide the fact that most people need supplemental folic acid to offset hidden toxins. Don’t be fooled, question the source of your nutrients.
Marcella Kennedy
October 28, 2025 AT 11:17When we talk about folate deficiency, it’s essential to consider not just the biochemical pathways but also the lived realities of those who navigate daily dietary constraints. Many individuals, especially those on strict plant‑based diets, assume that avoiding animal products automatically guarantees adequate micronutrient intake, yet the bioavailability of folate from certain sources can be surprisingly low. Moreover, socioeconomic factors often dictate access to fortified foods, which are a reliable source of synthetic folic acid that bypasses the intestinal conversion steps. Chronic alcohol consumption further complicates matters by impairing the intestinal mucosa, reducing folate absorption, and increasing renal excretion. Prescription medications such as anticonvulsants and methotrexate act as pharmacological antagonists, directly interfering with folate metabolism at the cellular level. Gastrointestinal disorders like celiac disease or Crohn’s disease bring another layer of malabsorption, rendering even a diet rich in leafy greens insufficient. Pregnant individuals face an amplified demand; the neural tube closure in the embryo occurs within the first few weeks, often before a pregnancy is confirmed, making preconception supplementation a public health priority. Genetic polymorphisms, particularly in the MTHFR gene, can diminish the conversion of dietary folate to its active methylated form, necessitating the use of methylfolate rather than standard folic acid. The clinical presentation-fatigue, glossitis, macrocytic anemia-can be subtle and easily mistaken for other conditions, delaying diagnosis and treatment. Laboratory assessment should therefore include both serum and red blood cell folate measurements to capture acute and chronic status, respectively, alongside homocysteine levels to gauge functional deficiency. Treatment protocols generally begin with a daily 400–800 µg of folic acid, escalating as needed based on severity and the presence of comorbidities. Ongoing monitoring every six to eight weeks ensures that hematologic parameters normalize and that homocysteine levels decline. Dietary counseling should emphasize a variety of folate‑rich foods-spinach, lentils, fortified cereals-while also addressing lifestyle factors like alcohol reduction. For patients with malabsorption syndromes, lifelong supplementation becomes a cornerstone of care, often requiring higher doses or the use of L‑methylfolate. Finally, public health initiatives must continue to fortify staple foods and educate at‑risk populations to close the gap between knowledge and practice. By integrating biochemical insight with practical, patient‑centered strategies, we can effectively combat folate deficiency and its far‑reaching consequences.
Jamie Hogan
November 2, 2025 AT 23:17Folate metabolism is a nuanced biochemical cascade that is often oversimplified in popular media. Understanding the enzymatic steps is crucial for effective intervention
Ram Dwivedi
November 8, 2025 AT 11:17Nice deep dive! 😊 I’d add that for people with MTHFR variants, taking 5‑MTHF can bypass the blocked step and improve outcomes quicker. Also, regular check‑ups keep you on track.
pooja shukla
November 13, 2025 AT 23:17All this “fortified grain” talk ignores the fact that our own country produces enough natural greens-stop buying foreign‑made supplements and support local farmers instead.
Poonam Mali
November 19, 2025 AT 11:17From a systems‑biology perspective, folate deficiency triggers a cascade of epigenetic dysregulation that can precipitate oncogenic pathways. The interplay between one‑carbon metabolism and methylation status is a critical node. Clinicians must therefore adopt a multimodal diagnostic algorithm. Ignoring these molecular intricacies is tantamount to malpractice.
Alan Whittaker
November 24, 2025 AT 23:17Don’t be fooled by “systems‑biology” buzzwords-the real issue is hidden pharma agendas that suppress natural folate sources to keep us dependent on patented supplements. Wake up.
Michael Waddington
November 30, 2025 AT 11:17Look, the data shows that most cases are just lifestyle choices. If you’re not eating beans, no wonder you’re low. Stop making excuses.
HAMZA JAAN
December 5, 2025 AT 23:17Wow, dropping the blame on personal choices is a classic deflection-maybe the real problem is the lack of accessible nutrition education in our communities?
April Rios
December 11, 2025 AT 11:17Philosophically speaking, folate represents the bridge between our material needs and existential health. When we neglect it, we undermine our capacity for both physical and metaphysical growth. The article rightly highlights this connection. However, the discourse often neglects the cultural dimensions of diet. Integrating tradition with science could yield richer solutions.
byron thierry
December 16, 2025 AT 23:17While the piece provides a thorough overview, it could benefit from a more detailed discussion on regional dietary variations. Nevertheless, the recommendations are sound and evidence‑based. I appreciate the balanced tone.
bob zika
December 22, 2025 AT 11:17Thank you for the comprehensive guide; it will be a valuable resource for patients. I look forward to sharing it with my colleagues.
M Black
December 27, 2025 AT 23:17Glad you liked it :) This kind of info really helps people take charge of their health
Sidney Wachira
January 2, 2026 AT 11:17Everyone acting like folate is a minor detail while the world burns-seriously, this is a cornerstone nutrient! 🤦♂️ If you ignore the signs, you risk anemia, birth defects, and even cardiovascular issues. It’s not just a “vitamin” but a life‑saver. Spread the word.
Aditya Satria
January 7, 2026 AT 23:17While enthusiasm is appreciated, let’s keep the discussion factual and free of exaggeration. Folate deficiency is common but manageable with proper diet and supplementation. Overstating the danger can cause unnecessary panic. Clear, calibrated messaging serves the community best.
Jocelyn Hansen
January 13, 2026 AT 11:17Great discussion, everyone! 😊 Remember, consistency with a balanced diet and regular check‑ups is key to staying ahead of deficiency. Keep supporting each other!