Fertomid (Clomiphene) vs Alternatives: Complete Comparison Guide
 Oct, 17 2025
Oct, 17 2025
Fertility Medication Decision Guide
Personalize Your Recommendation
When a couple’s journey to parenthood stalls, the first question often is: which ovulation‑inducing drug will give the best chance? Fertomid (the brand name for clomiphene citrate) has been the go‑to for decades, but newer options and older tricks are gaining ground. This guide breaks down how Fertomid works, who might benefit, and how it stacks up against the most common alternatives.
What is Fertomid (Clomiphene) and How Does It Work?
Fertomid is a selective estrogen receptor modulator (SERM) marketed primarily for ovulation induction. It binds to estrogen receptors in the hypothalamus, tricking the brain into thinking estrogen levels are low. This triggers a surge of gonadotropin‑releasing hormone (GnRH), which in turn boosts follicle‑stimulating hormone (FSH) and luteinizing hormone (LH) release from the pituitary. The result is accelerated follicular growth and a higher likelihood of ovulation.
The drug comes in 50mg tablets, typically started on day3‑5 of a natural menstrual cycle. Dosage is titrated up to 150mg per day based on response, and treatment is usually limited to six cycles to avoid ovarian hyperstimulation.
Top Alternatives to Fertomid
While Fertomid remains popular, several other agents can be more suitable depending on age, underlying diagnosis, and previous response.
- Letrozole is an aromatase inhibitor that lowers estrogen production, prompting the hypothalamus to increase GnRH output. It’s often preferred for women with polycystic ovary syndrome (PCOS) because it produces a thinner estrogen environment, reducing the risk of multiple pregnancies.
- Gonadotropins (e.g., urinary‑derived menotropin or recombinant FSH) are injectable hormones that directly stimulate the ovaries. They give the highest control over follicle development but require careful monitoring and are the most expensive option.
- Metformin is an insulin‑sensitizing agent used off‑label for ovulation induction in insulin‑resistant PCOS patients. It can be combined with other agents or used alone in milder cases.
- Tamoxifen is another SERM similar to clomiphene but with a slightly different receptor profile. It’s sometimes chosen when clomiphene fails or causes severe side effects.
- Anastrozole is a third‑generation aromatase inhibitor, less commonly used in fertility but occasionally preferred for its short half‑life and low multiple‑pregnancy rate.
Success Rates: How Effective Are the Options?
Clinical data give us a rough picture of how each drug performs in real‑world settings. Success is usually measured by ovulation (≈80‑90% for most agents) and live‑birth rates (≈15‑30% per cycle, varying by age and cause).
| Medication | Mechanism | Typical Dose (UK) | Ovulation Rate | Live‑Birth Rate per Cycle | Common Side Effects | Approx. Cost (per cycle) |
|---|---|---|---|---|---|---|
| Fertomid (Clomiphene) | SERM - blocks estrogen feedback | 50‑150mg daily, 5‑10days | ≈85% | 18‑22% | Hot flashes, mood swings, ovarian cysts | £30‑£50 |
| Letrozole | Aromatase inhibitor - reduces estrogen synthesis | 2.5‑5mg daily, 5days | ≈80% | 20‑24% | Fatigue, mild headache | £40‑£70 |
| Gonadotropins (FSH/hMG) | Direct ovarian stimulation | 75‑150 IU daily, 7‑10days | ≈95% | 25‑30% | Ovarian hyperstimulation, multiple pregnancy | £800‑£1500 |
| Metformin | Improves insulin sensitivity | 500‑1500mg daily | ≈70% | 12‑16% (often as adjunct) | GI upset, metallic taste | £20‑£35 |
| Tamoxifen | SERM - similar to clomiphene | 20‑40mg daily, 5‑10days | ≈80% | 15‑20% | Blurred vision, thrombo‑embolism risk (rare) | £45‑£80 |
Safety Profile and Side‑Effect Landscape
Every medication carries a risk‑benefit balance. Fertomid’s most cited concerns are hot flashes, mood swings, and a 5‑10% chance of developing functional ovarian cysts. Letrozole’s profile is generally milder, but rare cases of ovarian hyperstimulation have been reported, especially when combined with gonadotropins.
Injectable gonadotropins demand careful ultrasound monitoring because high estradiol levels can precipitate ovarian hyperstimulation syndrome (OHSS). The severity ranges from mild abdominal discomfort to life‑threatening fluid shifts, so physicians usually start with low doses and adjust based on follicular response.
Metformin’s gastrointestinal side effects (nausea, diarrhea) can be mitigated by a gradual titration and taking the dose with meals. Rarely, lactic acidosis is a concern, but it occurs mostly in patients with significant renal impairment.
Tamoxifen carries a small, though notable, increased risk of venous thromboembolism and, in very long‑term use, endometrial changes. Because fertility cycles are short, the absolute risk remains low.
Cost Considerations in the UK Context
Financial pressure is a real part of the decision. Fertomid and clomiphene are generic, making them the most affordable option-often covered by NHS prescriptions for certain indications. Letrozole is slightly pricier but still within a modest personal‑budget range.
Gonadotropins are the costliest tier. Even with NHS support for IVF cycles, the medication portion may require a private contribution. Many clinics offer “shared‑risk” funding schemes where the patient only pays if treatment fails, but the upfront out‑of‑pocket cost can still be steep.
Metformin is cheap, but its efficacy as a stand‑alone ovulation agent is limited to insulin‑resistant PCOS cases. Tamoxifen sits in the middle-more expensive than clomiphene but cheaper than injectable hormones.
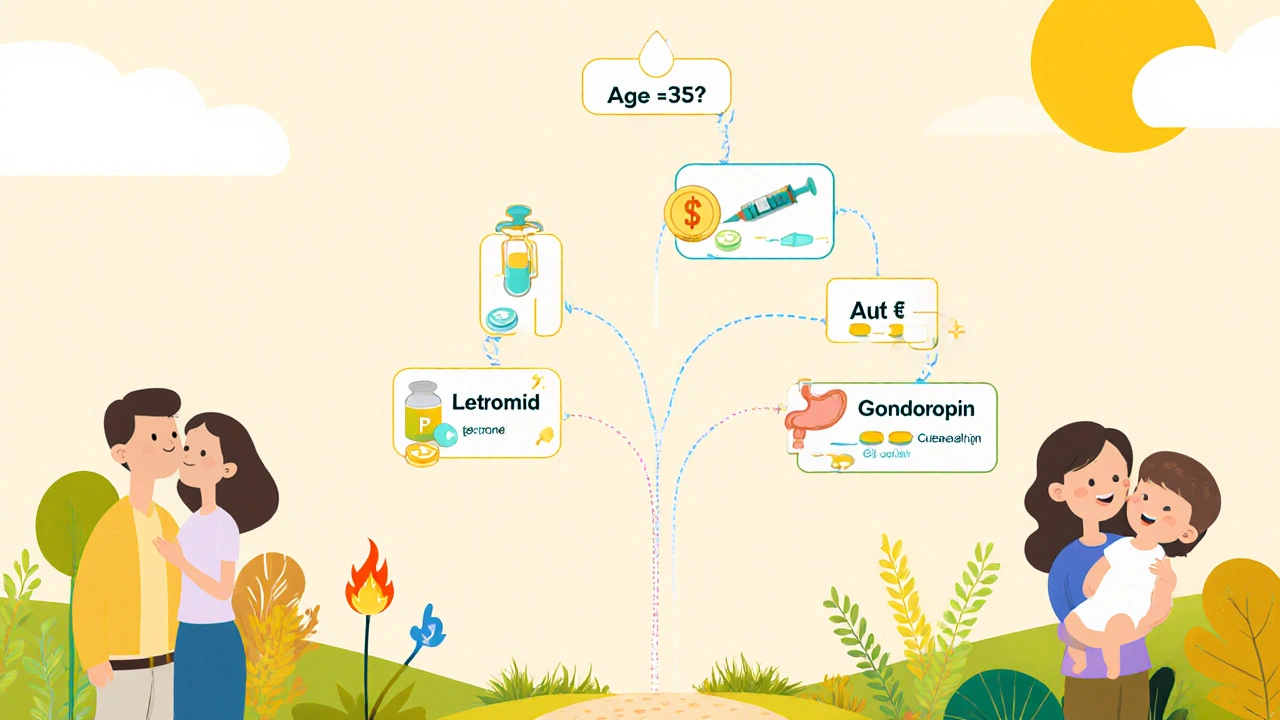
Choosing the Right Medication: A Decision Guide
Below is a quick decision tree to help you and your clinician land on the best choice.
- Are you under 35years old with a diagnosis of PCOS?
- Yes → Start with letrozole (2.5‑5mg) or clomiphene if letrozole unavailable.
- No → Consider fertility cause: if unexplained infertility, clomiphene remains first‑line.
- Have you failed two cycles of clomiphene?
- Yes → Switch to letrozole or add metformin (if insulin‑resistant).
- No → Continue clomiphene, adjusting dose up to 150mg.
- Do you have a high risk of multiple pregnancy or OHSS?
- Yes → Prefer letrozole or low‑dose gonadotropins with close monitoring.
- No → Gonadotropins can be considered for higher ovulation rates.
- Is cost a major constraint?
- Yes → clomiphene (Fertomid) or metformin are the most budget‑friendly.
- No → Gonadotropins or combination protocols can be explored.
Always discuss these steps with a fertility specialist who can tailor treatment to your hormone profile, ultrasound findings, and personal preferences.
Key Takeaways
- Fertomid (clomiphene) remains the cheapest, widely available first‑line agent.
- Letrozole often outperforms clomiphene in PCOS patients and carries a lower multiple‑pregnancy risk.
- Injectable gonadotropins give the highest ovulation and live‑birth rates but are expensive and need intensive monitoring.
- Metformin is a useful adjunct for insulin‑resistant cases; tamoxifen is a backup when clomiphene fails.
- Cost, age, infertility cause, and side‑effect tolerance should drive the final choice.
Frequently Asked Questions
Can I use Fertomid and Letrozole together?
Combining the two is generally not recommended because they act on the same hormonal pathway and can increase the risk of ovarian hyperstimulation without adding benefit. Most clinicians choose one or the other based on patient profile.
How long should I wait between cycles of Fertomid?
A typical wash‑out period is one full natural menstrual cycle (about 28days) to allow hormone levels to reset. Some doctors may shorten this if ovulation is confirmed and side effects are minimal.
What are the signs of ovarian hyperstimulation syndrome?
Early signs include rapid weight gain, abdominal bloating, nausea, and shortness of breath. Severe cases may involve painful swollen ovaries, decreased urine output, and fluid in the chest. Immediate medical attention is required if symptoms worsen.
Is Fertomid covered by the NHS?
Yes, clomiphene (including the brand Fertomid) can be prescribed on the NHS for specific infertility diagnoses, especially in women under 40 with anovulation. Eligibility varies by region, so check with your GP or fertility clinic.
When should I consider moving from oral agents to injectable gonadotropins?
If you’ve tried at least two cycles of oral medication (clomiphene or letrozole) without ovulation or pregnancy, or if your ovarian reserve is low and you need precise follicle control, a switch to injectable gonadotropins is usually advised.

kendra mukhia
October 17, 2025 AT 20:40Wow, this guide is a roller‑coaster of facts and drama! It feels like the author tried to cram every hormone shortcut into a single post, and honestly, some of it borders on medical mythology. While the tables are handy, the “six‑cycle limit” for Fertomid is a bit of a mythology tossed around by older textbooks. I’m convinced that if you’re under 30 and dealing with PCOS, Letrozole should be the first line-no debate. So, pick your poison wisely, but remember that cost isn’t the only villain here.
Bethany Torkelson
October 27, 2025 AT 01:54Enough with the sugar‑coating! These drugs aren’t just “poisons” you can pick casually, they’re life‑changing, and the pressure to choose the cheap option can ruin families. If a clinician pushes Fertomid just because it’s cheap, they’re betraying patients. Stop pretending it’s a simple decision and start caring about real outcomes.
Grace Hada
November 5, 2025 AT 08:07Facts are facts: letrozole outperforms clomiphene in PCOS, period.
alex montana
November 14, 2025 AT 14:20Well… you said that??! But… have you considered the rare ovarian cyst risk? It’s … not zero, and some women freak out!!
Sarah Hanson
November 23, 2025 AT 20:34In summary, clomiphene remains cost‑effective yet may requre careful monitoring.
Nhasala Joshi
December 3, 2025 AT 02:47Did you know the pharma giants are secretly funding the “low‑cost” clomiphene narrative? 🤔💊 They want us to ignore the hidden side‑effects while they line their pockets. Wake up, sheeple! 🚨
Wyatt Schwindt
December 12, 2025 AT 09:00I understand the stress of choosing a medication; many couples feel overwhelmed.
Lyle Mills
December 21, 2025 AT 15:14Exactly, the decision matrix can be noisy, but a thorough baseline work‑up-FSH, LH, AMH-helps narrow down the optimal protocol.
Barbara Grzegorzewska
December 30, 2025 AT 21:27Honestly, the whole discourse smells of populist oversimplification; an elite understanding of SERM pharmacodynamics reveals why Tamoxifen is the unsung hero for clomiphene‑resistant cases.
Nis Hansen
January 9, 2026 AT 03:40When we examine the landscape of ovulation induction, we must first acknowledge that fertility is not merely a biochemical cascade but a deeply personal narrative woven into each couple’s story. The pharmacologic agents listed-clomiphene, letrozole, gonadotropins, metformin, tamoxifen-each occupy a distinct niche on the therapeutic spectrum. Clomiphene’s legacy as the “first‑line” drug stems from its affordability and decades‑long clinical experience, yet its side‑effect profile, including mood swings and ovarian cysts, cannot be dismissed as trivial. Letrozole, by virtue of its aromatase inhibition, creates a thinner estrogen milieu, which statistically reduces the incidence of multiple gestations-an advantage for patients fearful of twins. Gonadotropins, while offering the highest ovulation rates, demand rigorous ultrasound monitoring to avert ovarian hyperstimulation syndrome, a potentially life‑threatening complication. Metformin’s role is less about direct ovulation induction and more about correcting insulin resistance, a cornerstone in many PCOS cases. Tamoxifen, though structurally akin to clomiphene, can bypass certain receptor resistance mechanisms, providing a valuable fallback. The cost gradient-from £30 for clomiphene to upwards of £1500 for gonadotropins-mirrors the intensity of medical supervision required for each. Moreover, the decision matrix must factor in patient age, ovarian reserve, and prior treatment failures to avoid unnecessary escalation. Clinical guidelines emphasize a stepwise approach, reserving injectable hormones for those who have exhausted oral options without success. From an ethical standpoint, we must also consider equitable access; the NHS subsidizes clomiphene, making it a pragmatic choice for many. However, insurance coverage for letrozole and gonadotropins varies, creating disparities that can influence outcomes. Ultimately, the “best” medication is not a one‑size‑fits‑all answer but a personalized prescription calibrated to physiological, financial, and emotional parameters. Couples should engage in candid discussions with their reproductive endocrinologist, weighing benefits against risks in a shared decision‑making process. In conclusion, knowledge empowers patients to navigate this complex terrain with confidence and hope.
Fabian Märkl
January 18, 2026 AT 09:54Great synthesis! 🙌 This helps me see the bigger picture without getting lost in jargon.
Avril Harrison
January 27, 2026 AT 16:07Interesting read-never realized how much the drug choice can affect both the wallet and the emotional roller‑coaster.
Natala Storczyk
February 5, 2026 AT 22:20THIS IS NOT A SIMPLE CHOICE; IT’S A LIFE‑ALTERING DECISION!!! DO NOT UNDERESTIMATE THE POWER OF HORMONES!!!