Electrolyte Imbalances: Managing Potassium, Phosphate, and Magnesium in Kidney Health
 Nov, 19 2025
Nov, 19 2025
Why Electrolyte Imbalances Matter More Than You Think
When your kidneys aren’t working right, your body’s balance of potassium, phosphate, and magnesium can slip out of control-fast. These aren’t just numbers on a lab report. They’re the silent conductors of your heartbeat, breathing, and muscle function. A potassium level below 3.0 mEq/L can trigger dangerous heart rhythms. A phosphate level under 1.0 mg/dL can leave you too weak to breathe on your own. And low magnesium? It doesn’t just cause cramps-it can make potassium replacement fail completely, even when you’re giving it straight into your vein.
These imbalances aren’t rare. In hospitals, especially with kidney disease or heart failure, they’re common. And they’re deadly if missed. The National Institute for Health and Care Excellence (NICE) issued safety alerts in 2021 and 2022 because too many patients were getting hurt by electrolyte errors. The good news? Most of these problems are preventable-if you know what to look for and when to act.
Normal Ranges and When to Worry
Here’s what normal looks like, and where things turn dangerous:
- Potassium: Normal is 3.2-5.0 mEq/L. Below 3.0? High risk for arrhythmias. Above 6.5? Emergency. Levels over 7.0 mEq/L with ECG changes mean you need treatment now.
- Magnesium: Normal is 1.7-2.2 mg/dL. Below 1.0 mg/dL? You’re in trouble. Above 2.5 mg/dL? Risk of muscle paralysis and stopped breathing.
- Phosphate: Normal is 2.5-4.5 mg/dL. Below 1.0 mg/dL? Respiratory failure can follow. Above 4.5 mg/dL? Can cause calcium to drop and lead to organ damage.
These aren’t just guidelines-they’re red flags. If you’re on dialysis, taking diuretics, or have advanced kidney disease, your levels need checking at least once a week. Outpatients on ACE inhibitors or SGLT2 inhibitors? Same rule applies. Don’t wait for symptoms. By the time you feel weak or your heart skips, it’s already late.
The Hidden Link: Why Magnesium Comes First
Here’s something most people get wrong: you can’t fix low potassium if magnesium is also low. It’s not a suggestion-it’s a rule. If your magnesium is under 1.7 mg/dL, giving potassium won’t work. Your kidneys just keep dumping it out, no matter how much you give.
Why? Magnesium is the key that unlocks potassium’s hold on your cells. Without enough magnesium, your body can’t reabsorb potassium properly. This is why hypokalemia that doesn’t respond to treatment is almost always hypomagnesemia in disguise.
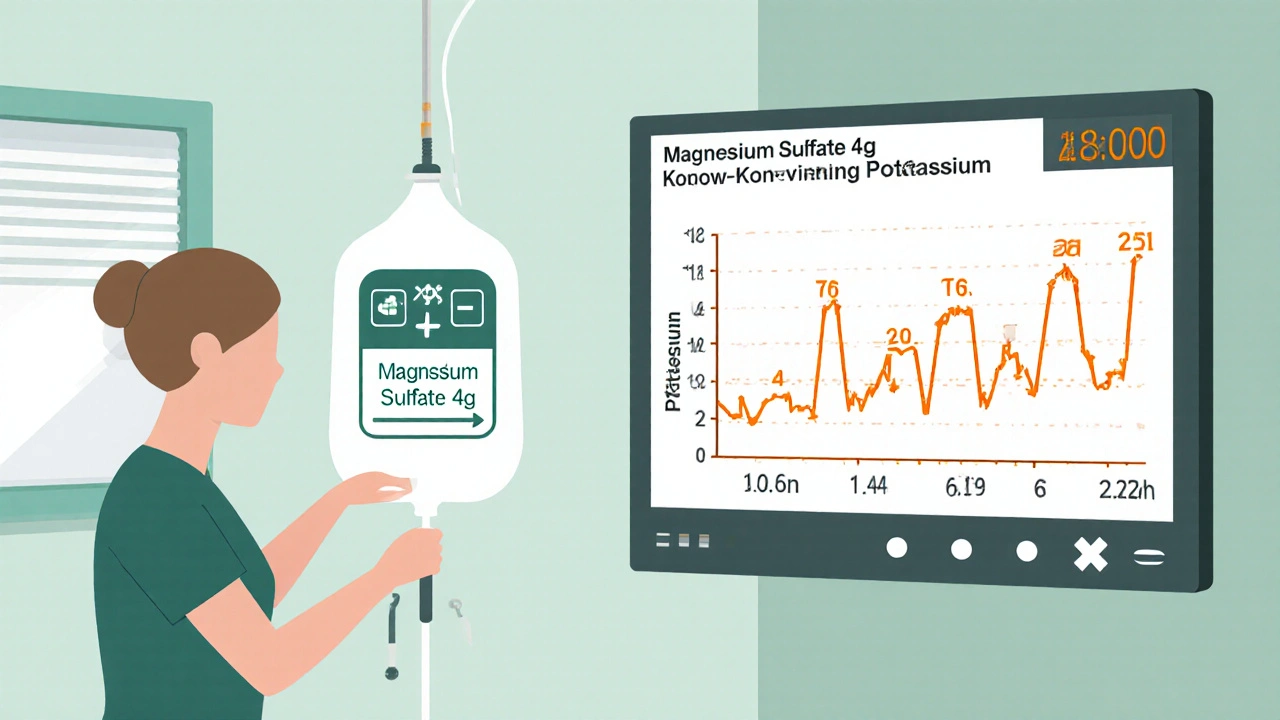
That’s why every hospital protocol-from Vanderbilt to the American Heart Association-says: check magnesium before you give potassium. If it’s low, replace it first. Standard dose? 4 grams of magnesium sulfate in 100 mL of fluid, infused over 30-60 minutes. Not fast. Not slow. Just right. Giving it too fast can drop your blood pressure. Too slow, and you’re wasting time.
And don’t forget: low magnesium often hides with low calcium. If you’re giving calcium to fix a low level, and magnesium is still low? The calcium won’t stick. You’ll need both.
Fixing High Potassium: The Emergency Playbook
High potassium is a ticking time bomb. It doesn’t always cause symptoms-until your heart stops. If your potassium is above 6.5 mEq/L, or you see peaked T-waves on your ECG, you’re in a code situation.
Here’s what happens next, in order:
- Calcium gluconate (10-20 mL of 10% solution): This doesn’t lower potassium. It protects your heart. It stabilizes the electrical membrane so your heart doesn’t fibrillate. Give it over 2-5 minutes. Effects last 30-60 minutes.
- Insulin and glucose: 10 units of regular insulin with 50 grams of dextrose (D50). This shifts potassium into your cells. Works in 15-30 minutes. Lasts 4-6 hours. Watch your blood sugar-this can crash it.
- Potassium binders: Patiromer or sodium zirconium cyclosilicate. These are newer, safer than old-school kayexalate. They grab potassium in your gut and flush it out. NICE approved them in January 2023. They’re not for emergencies-but for keeping levels down after the crisis.
- Dialysis: If you have kidney failure, or potassium won’t drop, dialysis is the only real fix. Don’t delay.
After treatment, check potassium again at 1, 2, 4, 6, and 24 hours. It can rebound. A lot of patients get discharged too soon and end up back in the ER.
Low Phosphate: The Silent Killer in ICU Patients
Phosphate doesn’t get enough attention. But in critically ill patients-especially those on ventilators or recovering from surgery-it’s a major risk. Low phosphate means your muscles, including your diaphragm, can’t contract. You can’t breathe. You need help.
Causes? Three big ones:
- Refeeding syndrome (when someone who’s starved starts eating again)
- Too many phosphate binders (common in kidney patients on dialysis)
- Ferric carboxymaltose-an IV iron drug the FDA flagged in 2020 for causing severe phosphate drops
Replacement depends on severity. If your phosphate is under 1.0 mg/dL, you need IV. Typical dose: 7.5 mmol in 250 mL of fluid over 4-6 hours. Don’t rush it. Too fast, and you can trigger low calcium, low magnesium, or even calcification of soft tissues.
Oral phosphate? 8 mmol per dose, 3-4 times a day. Works for mild cases. But if you’re in the ICU, IV is the only way to go. And always check magnesium and calcium when replacing phosphate-they’re all connected.
Hypermagnesemia: Rare, But Deadly
High magnesium is uncommon. Usually, it’s from too much antacid (like magnesium hydroxide), or kidney failure. But when it happens, it’s serious.
At 2.5-4 mg/dL: you feel sluggish, nauseous. At 4-6 mg/dL: your reflexes disappear. At 6+ mg/dL: you stop breathing. Your heart slows. You can die.
Treatment is simple, but urgent:
- Stop all magnesium sources-no Epsom salts, no antacids, no IV magnesium.
- Give 10-20 mL of calcium gluconate 10% IV. It reverses the muscle and nerve blockade.
- If your kidneys still work, give furosemide to flush it out.
- If you’re in kidney failure? Dialysis. No other option.
Don’t ignore symptoms. If someone on dialysis starts slurring their speech or can’t move their arms, check magnesium. It’s often the missing piece.
Monitoring: When and How Often
Checking electrolytes once a week isn’t enough if you’re high-risk. Here’s the real schedule:
- After treating hyperkalemia: Check potassium at 1, 2, 4, 6, and 24 hours. Rebound is common.
- During phosphate replacement: Check every 4-6 hours. Watch for rebound hyperphosphatemia.
- After magnesium replacement: Check at 4 and 12 hours. Levels can drop again.
- For all kidney patients: Monthly panel for potassium, phosphate, magnesium. More often if on diuretics or new meds.
Point-of-care testing in ERs now cuts time-to-treatment by 37 minutes. That’s huge. If you’re in a clinic or hospital, push for rapid electrolyte testing. Waiting 24 hours for lab results can kill.
What’s New in 2025
Things are changing fast. In 2023, the FDA approved new phosphate binders that don’t cause phosphate loss-big win for kidney patients. In 2024, phase 3 trials started for genetic tests that predict who’s likely to lose potassium on diuretics. Soon, we might tailor treatment based on your DNA.
Also, hospitals are using clinical decision support tools. If you’re prescribed a new diuretic or ACE inhibitor, the system auto-suggests an electrolyte check. Since 2021, teaching hospitals using these tools saw a 22.4% drop in electrolyte-related errors, according to JAMA Internal Medicine.
What You Can Do
If you have kidney disease:
- Know your numbers. Ask for your last potassium, magnesium, and phosphate levels every visit.
- Don’t take OTC antacids with magnesium unless your doctor says yes.
- If you’re on IV iron, ask if ferric carboxymaltose is the right choice. Ask about phosphate checks before and after.
- If you’re on dialysis, track your diet. Avoid high-potassium foods if your levels are high. Avoid high-phosphate foods if your levels are low.
- Speak up. If you feel weak, your heart races, or you’re dizzy-say it. Don’t wait.
Electrolyte imbalances aren’t mysterious. They’re predictable. And with the right checks and timing, they’re avoidable. Your kidneys are doing their job. The rest is up to you-and your care team.
Can low magnesium cause low potassium even if I’m taking potassium supplements?
Yes. Low magnesium makes your kidneys unable to hold onto potassium, no matter how much you take. This is called "refractory hypokalemia." You must correct magnesium first-usually with 4 grams IV-before potassium replacement will work. Many patients get stuck in a cycle of giving more potassium, seeing no change, and getting frustrated. The fix isn’t more potassium. It’s magnesium.
Why do I need to check calcium when treating low phosphate?
When you give phosphate, it binds to calcium in your blood, which can cause your calcium level to drop suddenly. This can lead to muscle spasms, seizures, or heart rhythm problems. Always check calcium before and after phosphate replacement. If calcium drops below 7 mg/dL, give calcium gluconate. This is standard in ICU protocols.
Is it safe to take oral magnesium supplements if I have kidney disease?
Only under doctor supervision. Kidneys normally clear excess magnesium. If your kidney function is low (eGFR under 30), you can’t clear it well. Oral magnesium can build up and cause toxicity-muscle weakness, low blood pressure, even breathing trouble. Stick to IV magnesium only if needed, and never self-prescribe supplements without testing your levels first.
What foods should I avoid if I have high potassium?
Avoid bananas, oranges, potatoes, tomatoes, spinach, beans, nuts, and salt substitutes (which often contain potassium chloride). Boiling vegetables can reduce their potassium by 50%. Stick to apples, cabbage, cauliflower, rice, and pasta. Always talk to a renal dietitian-what’s safe for one person isn’t safe for another.
Can diuretics cause all three electrolyte imbalances at once?
Yes. Loop diuretics like furosemide and thiazides cause potassium and magnesium loss. They also reduce phosphate reabsorption in the kidneys. Patients on long-term diuretics often have low potassium, low magnesium, and low phosphate simultaneously. That’s why monthly labs are non-negotiable. Many doctors miss this triple drop because they only check potassium.
What’s the difference between patiromer and sodium zirconium cyclosilicate?
Both bind potassium in the gut, but they work differently. Patiromer is a powder taken once daily, and it can cause constipation. Sodium zirconium cyclosilicate (brand name Lokelma) works faster-within hours-and is less likely to cause constipation. Both are safer than old potassium binders like kayexalate, which could cause bowel damage. NICE recommends both for long-term hyperkalemia control, especially if you’re on ACE inhibitors or ARBs.

Summer Joy
November 20, 2025 AT 11:36Aruna Urban Planner
November 20, 2025 AT 22:37Nicole Ziegler
November 21, 2025 AT 02:28Bharat Alasandi
November 22, 2025 AT 15:52Kristi Bennardo
November 23, 2025 AT 06:24Shiv Karan Singh
November 23, 2025 AT 21:19Ravi boy
November 24, 2025 AT 21:58Matthew Karrs
November 26, 2025 AT 10:23Dana Oralkhan
November 26, 2025 AT 23:06