Effective Tips for Managing Nausea During Chemotherapy
 Oct, 9 2025
Oct, 9 2025
Chemotherapy Nausea Management Planner
Select your regimen risk level and time since treatment to see personalized anti-emetic recommendations.
Select your regimen risk and time period to generate a customized daily checklist.
Explore effective non-pharmacologic methods to combat nausea.
Identify warning signs that require immediate medical attention.
One of the toughest side effects of cancer treatment is chemotherapy‑induced nausea is a common, often debilitating feeling of sickness that occurs during or after chemotherapy sessions. It can make eating, sleeping and daily activities a struggle, and if left unchecked it may even lead patients to miss vital treatment appointments. Managing chemotherapy nausea effectively can improve treatment tolerance and overall quality of life.
Key Takeaways
- Start anti‑nausea measures before the chemo session begins.
- Combine medication with non‑drug strategies for best results.
- Stay hydrated and eat small, bland meals throughout the day.
- Use ginger, acupressure, or relaxation techniques as safe, low‑cost helpers.
- Contact your medical team promptly if nausea worsens or you can’t keep fluids down.
What Causes Chemotherapy‑Induced Nausea?
The body’s reaction to chemo drugs triggers the brain’s vomiting centre, releasing chemicals like serotonin and substance P. These messengers tell the stomach to empty, leading to the queasy feeling. Different chemotherapy regimens have varying nausea potential; high‑emetic‑risk drugs such as cisplatin often cause stronger symptoms than low‑risk agents.

Non‑Pharmacologic Strategies That Work
While prescription anti‑emetics are powerful, pairing them with simple lifestyle tweaks can double the relief.
- Ginger is a natural anti‑nausea root that contains gingerol, which calms the stomach lining. Try ginger tea, candied ginger, or 1,000mg ginger capsules about an hour before chemo.
- Acupressure on the P6 (Neiguan) point-located three finger‑widths below the wrist-has shown a 30% reduction in nausea severity in several clinical trials. Wristbands are cheap and easy to wear.
- Stay hydrated with clear fluids (water, electrolyte drinks, broth) at a steady pace. Aim for 1500‑2000ml daily unless your doctor says otherwise.
- Eat small, frequent meals instead of three large ones. Bland foods like crackers, toast, bananas, rice and boiled potatoes are gentle on the stomach.
- Relaxation techniques such as deep‑breathing, guided imagery, or short mindfulness sessions can lower anxiety‑driven nausea spikes. Even five minutes before treatment helps.
Pharmacologic Options: A Quick Comparison
| Class | Typical Drug | How It Works | Best For | Common Side Effects |
|---|---|---|---|---|
| 5‑HT3 antagonists | Ondansetron | Blocks serotonin receptors in the gut and brain | d>Acute nausea (within 24h) | Headache, constipation |
| NK1 antagonists | Aprepitant | Blocks substanceP binding | Delayed nausea (24‑72h) | Fatigue, hiccups |
| Dopamine antagonists | Metoclopramide | Blocks dopamine receptors, promotes gastric emptying | Both acute & delayed | Drowsiness, muscle spasms |
| Corticosteroids | Dexamethasone | Anti‑inflammatory, reduces blood‑brain barrier permeability | Boosts other anti‑emetics | Increased appetite, insomnia |
| Natural remedies | Ginger, peppermint oil | Soothes gastrointestinal lining | Mild to moderate nausea | Rare, usually mild heartburn |
Putting It All Together: A Day‑by‑Day Checklist
- Night before chemo: Prepare ginger tea, pack a P6 wristband, and set reminders for medication.
- Morning of treatment: Drink 250ml of electrolyte water, eat a plain cracker, and take prescribed anti‑emetic (e.g., ondansetron) 30minutes before the infusion starts.
- During infusion: Keep the wristband on, practice slow diaphragmatic breaths (inhale for 4sec, exhale for 6sec), and sip water every 15minutes.
- Within 2hours post‑infusion: Have a small bowl of rice porridge or a banana, and consider a second dose of a delayed‑acting anti‑emetic (e.g., aprepitant) if prescribed.
- Evening: Relax with a guided meditation app for 10minutes, avoid strong smells, and log any nausea episodes in a symptom diary to share with your oncologist.
When to Call Your Medical Team
Even the best plan can hit snags. Reach out immediately if you experience any of the following:
- Persistent vomiting for more than 24hours.
- Inability to keep any fluids down, risking dehydration.
- Severe abdominal pain, fever, or diarrhea-signs of possible infection.
- Sudden onset of dizziness or fainting.
Prompt medical advice can prevent complications and may lead to adjustments in your medication regimen.
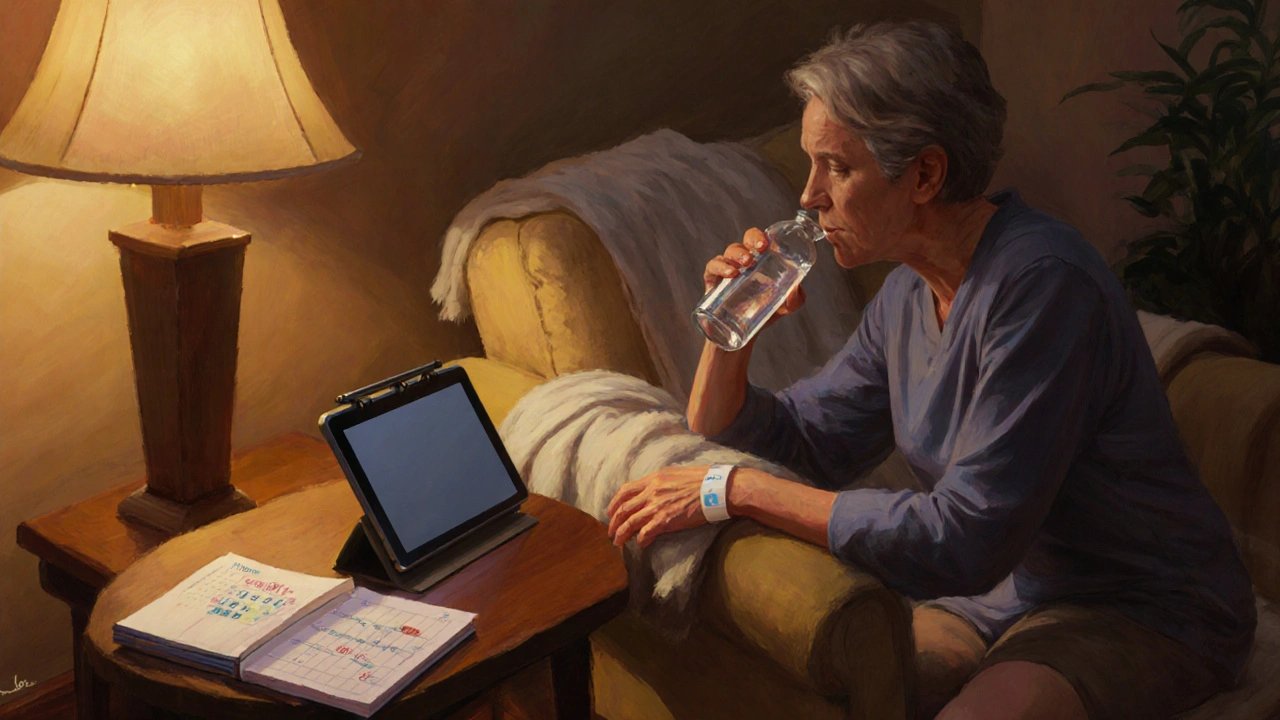
Supporting Caregivers: Tips to Lighten the Load
Family members and friends often become the on‑ground heroes. Here’s how they can help without burning out:
- Prepare a stash of bland snacks and keep them within easy reach.
- Set up a calm environment-soft lighting, minimal kitchen odors, and a comfortable seat for the patient.
- Track medication timing on a shared calendar app, so no dose is missed.
- Encourage short walks or gentle stretching if the patient feels up to it; movement can reduce nausea spikes.
- Take care of yourself-regular sleep, hydration, and a brief daily break keep you effective.
Frequently Asked Questions
Can I take over‑the‑counter ginger supplements during chemo?
Yes, most oncologists consider ginger safe in moderate amounts (up to 1g per day). However, check with your treatment team because high doses may interfere with blood‑thinning medications.
What’s the difference between acute and delayed chemotherapy nausea?
Acute nausea starts during or within the first 24hours after infusion, while delayed nausea peaks 24‑72hours later. Different anti‑emetic classes target each phase.
Is it okay to skip meals if I’m feeling nauseous?
Skipping meals can worsen nausea by leaving an empty stomach. Aim for small, bland bites every 2‑3hours. Liquids are especially important.
How do I know if my anti‑emetic dose needs adjustment?
If nausea persists despite taking the prescribed dose, or you experience side‑effects like severe constipation, discuss dosage changes with your oncologist. They may add a second drug or switch classes.
Can aromatherapy help with chemo nausea?
Mild scents such as peppermint or lemon can be soothing for some patients, but strong odors may trigger nausea in others. Test a small amount first and keep the room well‑ventilated.

isabel zurutuza
October 9, 2025 AT 21:07Wow another checklist for nausea because we all needed more paperwork
James Madrid
October 10, 2025 AT 13:47Hey that checklist actually looks solid; starting anti‑nausea steps before chemo can make a huge difference, especially when you stick to the small‑meal rule and keep hydration up.
Justin Valois
October 11, 2025 AT 06:27Listen up folks, the real hero here isn’t the ginger, it’s the mighty P6 wristband-like a medieval talisman that shields you from the evil chemo dragon! If you don’t strap that thing on, you might as well bring a spoon to a gunfight.
Jessica Simpson
October 11, 2025 AT 23:07In many Asian families, the ritual of sipping warm ginger tea before any major medical procedure is passed down for generations, and it’s amazing how that simple habit lines up perfectly with the anti‑nausea advice in this guide.
Ryan Smith
October 12, 2025 AT 15:47Sure, the pharma companies love you to have a "personalized plan" so they can push the newest anti‑emetic brand straight to your bedside while they keep the real cure hidden.
John Carruth
October 13, 2025 AT 08:27Honestly, I think the best thing you can do is treat this plan as a daily ritual rather than a checklist. The first step-pre‑treatment hydration-sets the tone for the whole day. When you sip water steadily instead of gulping, you give your stomach a chance to settle. Pair that with a modest amount of ginger, and you’ve already cut the odds of a violent bout in half. The next item, taking your anti‑emetic on schedule, is non‑negotiable; the timing is calibrated to hit the serotonin receptors before they get a chance to trigger nausea. After that, the P6 acupressure wristband is not just a gimmick; it provides a constant sensory cue that can distract the brain’s vomiting centre. Small, bland meals are emphasised for a reason-high‑fat or spicy foods can exacerbate the chemotoxic insult on the gut lining. Keep a symptom diary; writing down the exact time and severity of any nausea helps your oncologist fine‑tune doses. If you notice a pattern, don’t wait-call the clinic early. The meditation segment might sound cheesy, but a five‑minute mindfulness break can lower cortisol, which in turn reduces the nausea cascade. Remember to avoid strong odors; a whiff of perfume can be enough to trigger the reflex. If you’re feeling anxious, practice diaphragmatic breathing: inhale for four seconds, exhale for six, repeat. Finally, celebrate each small victory-whether it’s a full breakfast or a night of uninterrupted sleep. The cumulative effect of these tiny wins is a dramatically improved quality of life. And if any of these steps feel overwhelming, break them down further; the goal is consistency, not perfection. Keep at it, and you’ll find that chemo becomes a challenge you can manage rather than a nightmare you can’t escape.
Melodi Young
October 14, 2025 AT 01:07Okay love the enthusiasm but you don’t need to write a novel-just follow the checklist and you’ll be fine.
Tanna Dunlap
October 14, 2025 AT 17:47It’s ethically unacceptable to downplay nausea; patients suffering in silence while we hand them a list of tips is a betrayal of our duty to care.
Troy Freund
October 15, 2025 AT 10:27When you consider nausea as a signal rather than an enemy, the whole approach shifts from fighting to listening, and that mental pivot can soften the experience considerably.
Mauricio Banvard
October 16, 2025 AT 03:07Did you know some of those “natural” ginger capsules are actually laced with micro‑doses of stimulants to keep you jittery and buying more meds?
Paul Hughes
October 16, 2025 AT 19:47I get the skepticism but the wristband trick really does the job 😊 keep sipping water and you’ll notice the difference.
Mary Latham
October 17, 2025 AT 12:27Honestly i think the whole "drink 250ml of electrolyte water" thing is kinda overkill for most people.
Marie Green
October 18, 2025 AT 05:07I hear you – it can feel overwhelming, so try to focus on just one step at a time and remember you’re not alone in this.
TOM PAUL
October 18, 2025 AT 21:47You’ve got this! Every small bite, every breath, every wristband snap is a victory against the nausea beast.
Ash Charles
October 19, 2025 AT 14:27Don’t waste any time-grab that ginger, strap that band, and dominate that chemo session like a champ!
Michael GOUFIER
October 20, 2025 AT 07:07It is imperative that patients adhere strictly to the recommended anti‑emetic schedule, ensuring administration of ondansetron thirty minutes prior to infusion, followed by aprepitant as indicated for delayed onset, thereby optimizing therapeutic efficacy.
debashis chakravarty
October 20, 2025 AT 23:47While the article provides a commendable overview, it regrettably omits discussion of the pharmacogenomic variations that influence anti‑emetic metabolism, a glaring oversight for a comprehensive management plan.
Sara Blanchard
October 21, 2025 AT 16:27Remember that each person’s response is unique; fostering a supportive environment where caregivers share their own coping strategies can empower the entire treatment journey.
Anthony Palmowski
October 22, 2025 AT 09:07This guide is riddled with buzzwords-ginger, acupressure, hydration-yet fails to address the underlying psychosocial support deficits!!!