ECG and Stress Tests: What You Need to Know About Heart Diagnostic Tests
 Dec, 8 2025
Dec, 8 2025
When your doctor says you need an ECG or a stress test, it’s not because they’re being overly cautious. It’s because these tests can catch problems your heart won’t tell you about-until it’s too late.
What an ECG Actually Shows
An electrocardiogram, or ECG (sometimes called an EKG), is a simple, painless test that records your heart’s electrical signals. It doesn’t measure blood flow or pumping strength. It watches how electricity moves through your heart muscle. That’s important because when that electrical pattern gets messy, it can mean trouble.
During an ECG, ten small sensors stick to your chest, arms, and legs. They don’t shock you. They just listen. In about five minutes, you get a graph of spikes and dips that show your heart’s rhythm, speed, and timing. Doctors look for signs like irregular beats, past heart attacks, or blocked arteries. A normal ECG doesn’t mean your heart is perfect-but an abnormal one tells you something’s off.
For example, if your ECG shows a dip in the ST segment, that could mean your heart muscle isn’t getting enough oxygen. That’s a red flag for coronary artery disease. But here’s the catch: nearly 40% of people with early heart disease have a normal resting ECG. That’s why doctors often need more than just this test.
Why Stress Tests Exist
Your heart at rest is like a car idling in the driveway. It’s not working hard. But when you climb stairs, run, or even walk fast, your heart has to pump harder. That’s when problems show up.
A stress test forces your heart to work harder-either by making you walk on a treadmill or by giving you medicine that mimics exercise. The goal? To see how your heart handles pressure. If your arteries are narrowed from plaque, they can’t deliver enough blood when your heart demands more. That’s when chest pain, fatigue, or abnormal ECG changes appear.
Stress tests are especially useful for people with chest discomfort, shortness of breath during activity, or risk factors like high blood pressure, diabetes, or a family history of heart disease. The American College of Cardiology recommends them as the first step for people with a 15% to 65% chance of having coronary artery disease.
How a Treadmill Stress Test Works
The most common type is the exercise stress test using the Bruce Protocol. You start walking slowly on a treadmill, then every three minutes, it gets steeper and faster. By the end, you’re climbing like you’re scaling a hill at a brisk pace.
Throughout, your heart rate, blood pressure, and ECG are monitored. You’re asked to report any symptoms: chest tightness, dizziness, leg fatigue. The test stops when you reach 85% of your maximum heart rate (220 minus your age), or if you get too tired or symptomatic.
Most people last 6 to 12 minutes. That’s not a race-it’s a diagnostic tool. Each extra minute you walk lowers your risk of a future heart event by about 12%. If you can’t make it past 5 minutes, that’s a warning sign.
One Reddit user, CardiacWarrior87, said his treadmill test caught silent ischemia his resting ECG missed. He was 48, active, no symptoms-until the test showed his heart wasn’t getting enough blood under stress.
What If You Can’t Exercise?
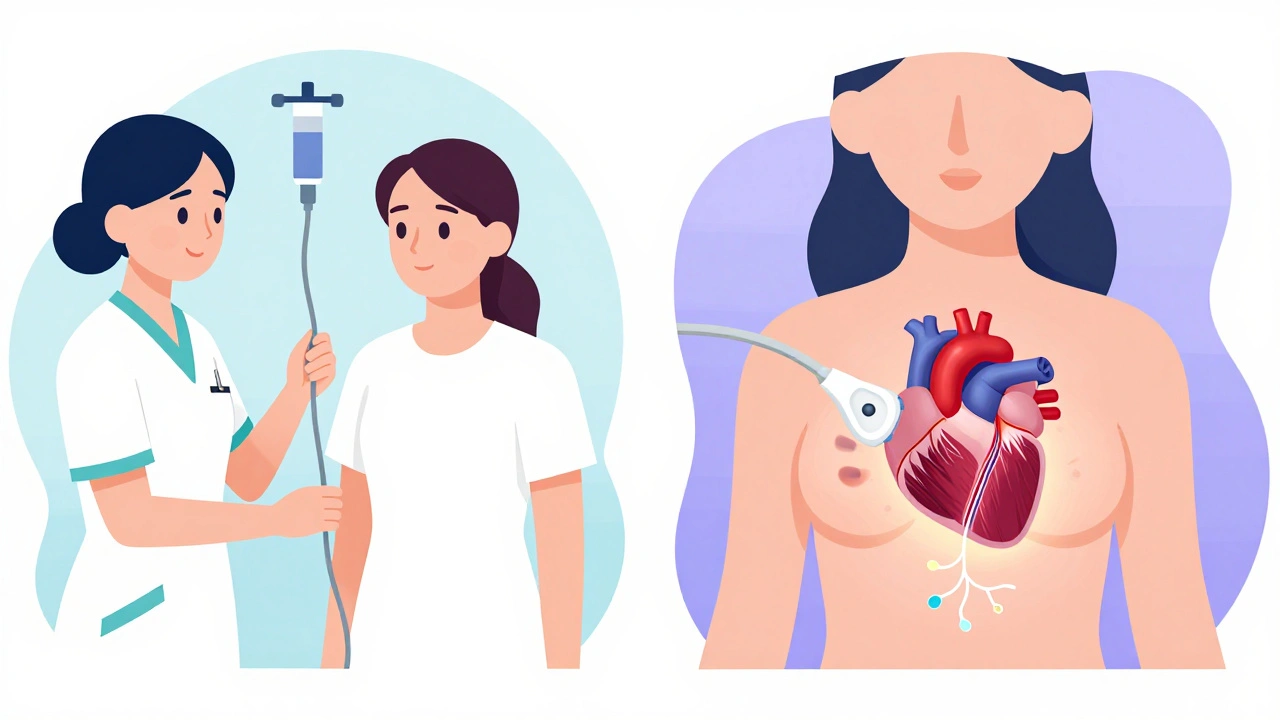
Not everyone can walk on a treadmill. Arthritis, lung disease, or recent surgery can make it impossible. That’s where chemical stress tests come in.
Instead of moving your body, doctors use drugs like adenosine or dobutamine to make your heart beat faster and harder. Adenosine opens blood vessels in healthy areas but not in blocked ones, creating a contrast. Dobutamine makes your heart pump harder, like exercise.
The side effects? Some people feel hot, short of breath, or get chest pressure. One patient on HealthUnlocked said it felt like she was dying for three minutes-but the nurse said it was normal. It passes quickly.
These tests take longer-up to an hour-and require more monitoring. But they’re safe for people who can’t move. The key is knowing your limits before you walk in.
Stress Echo vs. Nuclear Test: Which Is Better?
Not all stress tests are the same. There are two advanced versions that add imaging.
Stress echocardiography uses ultrasound to take pictures of your heart before and after stress. Doctors watch for parts of the heart that don’t move well under strain. That’s a sign of blocked arteries. This test has no radiation, costs about $514, and is more accurate than a plain stress ECG-especially in women.
Nuclear stress tests inject a tiny amount of radioactive tracer (like technetium-99m) and use a special camera to see blood flow in your heart. It’s more sensitive-it catches 85% of blockages-but you’re exposed to radiation equal to 3-4 years of natural background exposure.
Here’s the trade-off: Nuclear tests are better at finding problems, but stress echo is safer and just as good for many people. The American College of Cardiology now recommends stress echo as the first choice for middle-aged women with symptoms and intermediate risk. Why? Because women’s heart disease often affects tiny vessels, not big arteries-and echo picks that up better.
What the Numbers Really Mean
Let’s talk accuracy. A standard ECG stress test catches about 68% of coronary artery disease cases. That means nearly 1 in 3 people with blockages get a false negative. That’s especially true for women under 50. Their symptoms can be subtle-fatigue, nausea, jaw pain-not classic chest pain. And their arteries may be smaller, with different patterns of blockage.
Stress echo improves specificity to 88%, meaning fewer false alarms. Nuclear tests are more sensitive (89%) but less specific (79%), so they sometimes flag healthy hearts as problematic.
And cost? A CT scan of your heart runs about $404. Stress echo is $110 more. Nuclear stress tests? Nearly $950. The PROMISE trial found no big difference in long-term costs between these tests. So the cheapest isn’t always the best.
What You Should Do Before the Test
Don’t show up for a stress test with a coffee in hand. Caffeine interferes with the drugs used in chemical stress tests. Avoid coffee, tea, soda, chocolate, and energy drinks for 24 hours before.
Wear comfortable clothes and walking shoes. No dresses, no heels, no tight shirts. You’ll be moving. You’ll sweat. You’ll be asked to remove your shirt (for the ECG leads), so a button-up helps.
Fasting isn’t always required, but if you’re having a nuclear test, you might be told not to eat for 4-6 hours. Always check with the clinic.
Bring a list of your meds. Some drugs-like beta blockers or nitrates-can affect results. Your doctor may ask you to skip them the day of the test.
What Happens After?
Most people walk out right after. No recovery time. No sedation. You can drive, eat, and go back to work.
Results aren’t always instant. Some clinics give a quick readout before you leave. Others send a full report to your doctor in a few days. If your test shows a problem, you’ll likely be referred for a cardiac specialist or further imaging.
Even if your test is normal, don’t ignore symptoms. A clean ECG doesn’t mean you’re heart-safe forever. Lifestyle matters more than any test. Quit smoking. Move daily. Eat real food. Control your blood pressure and sugar.
What’s Changing in Cardiac Testing
Technology is making these tests smarter. Artificial intelligence now helps interpret ECG patterns during stress tests with 18-22% greater accuracy than human eyes alone. New portable devices, like the FDA-cleared Cardiac Dynamics StressPal, let clinics do stress tests in doctor’s offices or even nursing homes.
At Stanford, researchers are using advanced ultrasound techniques to spot microvascular disease in women-problems that used to be missed. This could change how we diagnose heart disease in half the population who’ve been told their symptoms were “just anxiety.”
By 2030, stress tests will still be a first-line tool-but their role may shrink for low-risk patients. As CT scans get cheaper and faster, they might replace stress tests for some. But for most people with symptoms, the treadmill or the drug test will still be the starting point.
When Not to Get a Stress Test
Stress tests aren’t for everyone. The European Society of Cardiology says avoid them if you’ve had a heart attack in the last 48 hours, have unstable heart rhythms, or are in acute heart failure. The risk of triggering a bad event is too high.
And don’t get one just because you’re worried. If you’re young, healthy, and have no symptoms, a stress test won’t help. It might even hurt-by leading to unnecessary follow-ups, anxiety, or even invasive procedures.
These tests are for people with symptoms or clear risk factors. Not for checkups. Not for peace of mind. For diagnosis.
Is an ECG the same as a stress test?
No. An ECG records your heart’s electrical activity while you’re at rest. A stress test monitors your heart while it’s under physical or chemical stress. A stress test often includes an ECG, but it adds movement or medication to see how your heart responds. One shows what your heart does when idle; the other shows what it does when working hard.
Can a stress test miss heart disease?
Yes. A standard exercise ECG stress test misses about 32% of coronary artery disease cases. False negatives are more common in women, especially those under 50, because their heart disease often affects small vessels, not the main arteries. Stress echocardiography or nuclear tests are more accurate, but even those aren’t perfect. Symptoms matter as much as test results.
Are stress tests dangerous?
They’re very safe when done properly. Serious complications like heart attack or dangerous arrhythmias happen in fewer than 1 in 1,000 tests. Medical staff are trained to stop the test and respond immediately if something goes wrong. The risk of not testing-missing a serious problem-is far greater than the risk of the test itself.
How long does a stress test take?
The actual exercise part lasts 10-15 minutes. But the whole process-including setup, monitoring, and recovery-takes about 45 to 60 minutes. Chemical stress tests take longer, up to 90 minutes, because the drugs need time to work and your heart needs to be monitored after the dose.
Do I need a referral for a stress test?
Yes. Stress tests are diagnostic tools, not routine screenings. You need a doctor’s order based on your symptoms, risk factors, or abnormal findings from other tests. You can’t just walk in and ask for one. Insurance typically requires a documented medical reason.
Can I eat or drink before a stress test?
Avoid caffeine for 24 hours before the test-it can interfere with the drugs used in chemical stress tests. You may be asked not to eat for 4-6 hours if you’re having a nuclear stress test. Always follow the specific instructions from your clinic. Drink water unless told otherwise.
What if my stress test is inconclusive?
About 25% of intermediate-risk patients get inconclusive results. That means the test didn’t clearly show whether there’s a blockage. The next step is usually a stress echocardiogram or a CT angiogram. Don’t panic. Inconclusive doesn’t mean abnormal-it means more information is needed. Your doctor will guide you on what to do next.
Bottom Line
ECGs and stress tests aren’t scary. They’re tools. Simple. Safe. Powerful. They don’t replace a healthy lifestyle-but they can catch problems before they become emergencies. If you have symptoms, don’t brush them off. If you’re at risk, ask your doctor. And if you’re told you need one, know this: it’s not about fear. It’s about knowing.

Taya Rtichsheva
December 10, 2025 AT 10:27so i got an ekg last year and the doc said im fine but then i passed out biking and turned out i had a blockage lol
Evelyn Pastrana
December 11, 2025 AT 18:44my grandma did a stress test and cried because she thought the machine was trying to kill her. the nurse had to hold her hand. she walked 8 minutes and lived to 92. also she still eats pie every sunday. heart health is just life with better shoes
Nikhil Pattni
December 11, 2025 AT 23:31yo you guys dont get it the real issue is that american doctors overtest everything because theyre scared of lawsuits. in india we just ask if you feel pain and if you say no we say you fine. no machines no stress no money. also i did a stress test once and the machine beeped so loud i thought it was my heart exploding. turns out i just had caffeine. lol. btw if you want real heart health drink turmeric milk and stop eating bread. also dont trust ai ekg readings theyre trained on white people data. my cousin got misdiagnosed because his rhythm looked "weird" but he was just indian. also i read a paper on pubmed that says...
Elliot Barrett
December 12, 2025 AT 19:41why are we even doing this? just get a ct scan and be done with it. this treadmill nonsense is a scam. they make you sweat for an hour so they can charge you $900. i did it once. got zero results. just a sweaty shirt and a bill. waste of time.
Andrea Beilstein
December 12, 2025 AT 22:58we treat the heart like a machine you fix when it breaks but its more like a song. sometimes the notes are off not because the instrument is broken but because the room is too loud or the singer is tired. the test just tells you the melody is wrong not why. maybe we should ask what the heart is trying to say before we force it to run on a treadmill
Sabrina Thurn
December 13, 2025 AT 08:28important note: stress echo is superior for microvascular dysfunction, which is underdiagnosed in women due to historical bias in cardiac research. the 2023 AHA guidelines now classify it as a class 1 recommendation for symptomatic women with intermediate risk. nuclear stress tests have higher sensitivity but lower specificity - meaning more false positives leading to unnecessary cath lab referrals. cost-effectiveness analysis from the PROMISE trial supports stress echo as first-line for this cohort. also, don't forget to hydrate and avoid NSAIDs 48h pre-test - they can blunt ischemic response. if you're anxious, breathe slow - the test is safer than driving to the clinic.
Richard Eite
December 14, 2025 AT 08:34usa is weak. we used to just run up hills and if you died you were weak. no tests no machines. if your heart can't handle a real workout you dont deserve to live. also caffeine is for cowards. just drink black coffee and run. problem solved.
Tim Tinh
December 15, 2025 AT 09:47my buddy had a stress test last month and he was so nervous he forgot to skip coffee. ended up getting a false positive and had to do a nuclear test. he was terrified. but turns out he was fine. just caffeine and anxiety. so if you're gonna do this? chill out. wear comfy clothes. bring your favorite playlist. they're not trying to break you. they're trying to help you live longer. also i always bring a banana after. because science.