Clindamycin and C. difficile Risk: When to Seek Care
 Nov, 12 2025
Nov, 12 2025
C. difficile Risk Assessment Tool
C. difficile Risk Assessment
Do you have any of these symptoms?
Risk Assessment Result
When you take clindamycin for a tooth infection, skin abscess, or other bacterial issue, you expect relief-not a dangerous gut infection. But here’s the hard truth: clindamycin is one of the riskiest antibiotics when it comes to triggering C. difficile (Clostridioides difficile), a bacterium that can turn mild diarrhea into a life-threatening condition. Even one dose can be enough. If you’re on clindamycin or just finished a course, knowing what symptoms to watch for-and when to act-could save your life.
Why Clindamycin Is So Dangerous for Your Gut
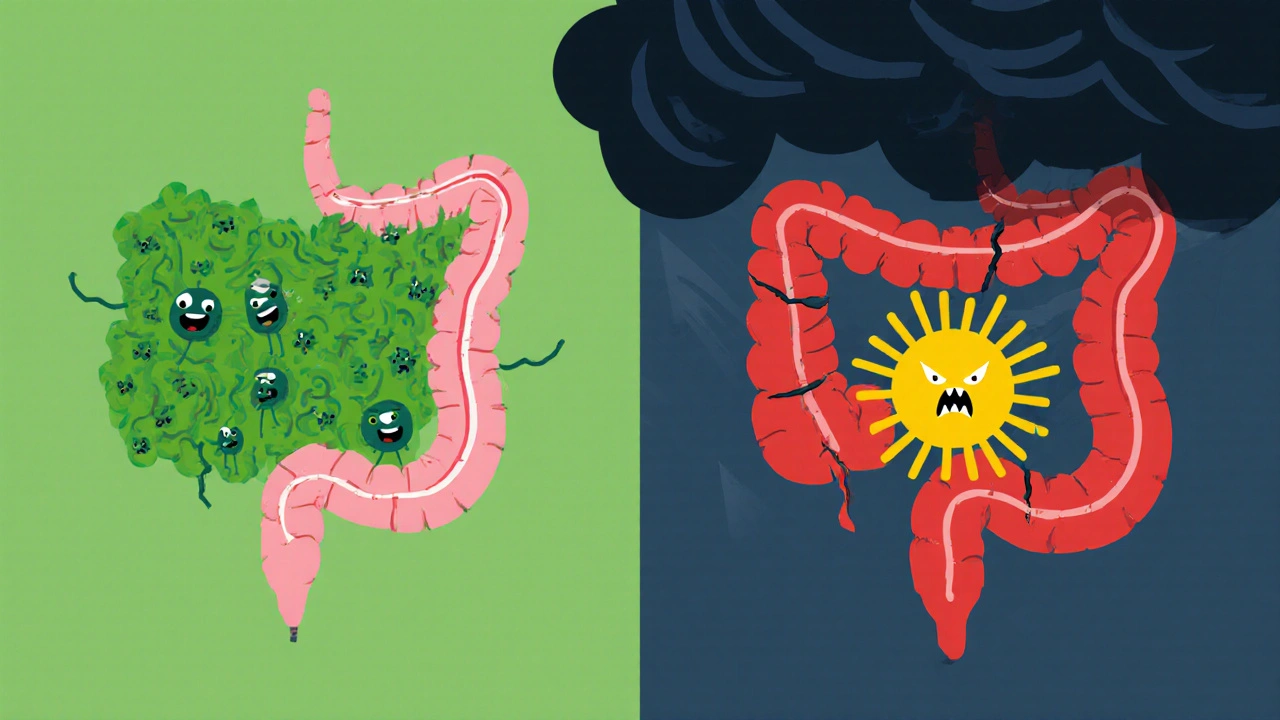
Not all antibiotics are created equal. Some, like doxycycline, barely touch your gut bacteria. Others, like clindamycin, wipe out entire neighborhoods of good bacteria in your intestines. Clindamycin targets gram-positive bacteria, which sounds fine until you realize those include the friendly bugs that keep C. difficile in check. Without them, C. difficile multiplies like wildfire and releases toxins that eat through the lining of your colon. Studies show clindamycin carries the highest risk of causing C. difficile infection (CDI) among all common antibiotics. A 2019 analysis of over 150,000 patients found clindamycin users were far more likely to develop CDI than those taking other drugs-even compared to other high-risk antibiotics like cephalosporins or fluoroquinolones. The reason? Clindamycin sticks around in your gut longer than most antibiotics, giving C. difficile more time to take over. And it’s not just hospital patients. About 20% of all CDI cases now start in the community, often after someone takes clindamycin for a dental infection or a skin rash. The CDC now lists clindamycin as a top contributor to this growing public health threat.What Does C. difficile Actually Do to You?
C. difficile doesn’t just give you loose stools. It causes inflammation so severe it can lead to pseudomembranous colitis-patches of dead tissue and pus lining your colon. Symptoms start mild but can spiral fast:- Three or more unformed stools in a single day
- Abdominal cramping or pain that doesn’t go away
- Fever above 101.3°F (38.5°C)
- Blood or pus in your stool
- Feeling dizzy, weak, or extremely thirsty (signs of dehydration)
- Swollen belly, no gas, or no bowel movements-this can mean your colon is shutting down
When Should You Seek Care? The Exact Signs
You don’t need to wait until you’re vomiting or passing blood. If you’re taking clindamycin-or if you’ve finished it within the last 12 weeks-and you notice any of these, call your doctor right away:- Two or more loose stools in 24 hours, especially if you also have cramps
- Any diarrhea that starts within 12 weeks of finishing antibiotics
- Any fever, even a low-grade one, along with diarrhea
- Signs of dehydration: dark urine, dry mouth, dizziness when standing
How Soon After Taking Clindamycin Can C. difficile Show Up?
Most people assume symptoms appear during treatment. But here’s the surprise: nearly half of clindamycin-related CDI cases show up after you’ve stopped taking it. The average time from starting clindamycin to symptoms is 5-10 days, but it can happen anytime from 1 day to 12 weeks later. A 2022 study of over 150,000 CDI cases found:- 22% of cases happened while still on clindamycin
- 46% appeared within one week of stopping
- 68% occurred within 14 days of starting the drug
What Happens If You Go to the Doctor?
Your doctor won’t just guess. They’ll test your stool for C. difficile toxins using a PCR test or enzyme immunoassay. If it’s positive, treatment starts immediately. For mild cases, they’ll stop clindamycin and prescribe metronidazole or vancomycin. For severe cases, they’ll use fidaxomicin or even IV antibiotics. If you’ve had C. difficile before, your doctor might recommend VOWST-a new FDA-approved treatment made of bacterial spores that helps rebuild your gut microbiome. It’s not a cure for active infection, but it cuts recurrence risk by 37% if given early. In extreme cases-like if you have low blood pressure, a swollen belly, or no bowel movements-you’ll be rushed to the hospital. Surgery to remove part of the colon may be needed if your colon is about to burst.
What Can You Do to Lower Your Risk?
The best way to avoid C. difficile is to avoid unnecessary antibiotics. But if you need clindamycin-for example, if you’re allergic to penicillin and have a serious skin or dental infection-talk to your doctor about alternatives. Ask:- Is there a lower-risk antibiotic that would work just as well?
- Could trimethoprim-sulfamethoxazole or a different class of drug be used instead?
- Is this dose really necessary? Sometimes, shorter courses are just as effective.
Why This Matters More Than You Think
C. difficile isn’t just a personal health issue-it’s a financial and systemic crisis. Each case costs an average of $13,500 in the U.S. because of longer hospital stays, ICU care, and surgeries. And the problem is growing. While hospital-acquired cases have dropped since 2017, community cases are rising-especially linked to outpatient antibiotic use. Dentists prescribe clindamycin more than any other antibiotic for penicillin-allergic patients. In fact, 13% of community CDI cases may be tied to dental prescriptions. That’s why the FDA now requires all antibiotic labels to clearly state CDI risk. Clindamycin’s label says it’s in the highest-risk category. Research is moving fast. New drugs like ridinilazole are showing promise in reducing recurrence rates by over 40% in patients exposed to clindamycin. But until those are widely available, awareness is your best defense.What to Do Right Now
If you’re currently on clindamycin:- Write down your bowel habits daily
- Watch for cramps, fever, or changes in stool
- Don’t ignore symptoms just because you’re still taking the medicine
- Still monitor for diarrhea
- Call your doctor if you have two or more loose stools in a day
- Don’t wait for it to get worse
Can you get C. difficile from a single dose of clindamycin?
Yes. Even one dose of clindamycin can trigger C. difficile infection in susceptible people. Case reports show CDI developing after a single pre-surgical dose. While the absolute risk is low (1-2% of courses), the danger is real because the toxin production can be rapid and severe.
How long after stopping clindamycin can C. difficile symptoms appear?
Symptoms can appear anytime from 1 day to 12 weeks after finishing clindamycin. Most cases (68%) show up within 14 days of starting the drug, and nearly half occur within a week of stopping. This long window means you’re not safe just because you’re off the antibiotic.
Is C. difficile contagious?
Yes. C. difficile spreads through spores in feces. These spores can survive on surfaces like toilets, doorknobs, and medical equipment for months. If someone touches a contaminated surface and then touches their mouth, they can become infected. Good handwashing with soap and water (not just hand sanitizer) is critical to prevent spread.
Can you get C. difficile without taking antibiotics?
It’s rare, but possible. People with weakened immune systems, those on long-term proton pump inhibitors, or those with severe underlying illness can develop CDI without recent antibiotic use. However, over 95% of cases are linked to antibiotics, with clindamycin being the most common trigger.
Should I take probiotics to prevent C. difficile while on clindamycin?
Evidence is mixed. Some studies suggest certain strains like Saccharomyces boulardii may help reduce risk, but others show no benefit. The CDC and major medical societies do not currently recommend probiotics as a standard prevention method. The best approach is to avoid unnecessary antibiotics and monitor symptoms closely.
What’s the difference between C. difficile and regular diarrhea?
Regular diarrhea from food poisoning or a virus usually lasts 1-2 days and resolves on its own. C. difficile diarrhea is persistent (three or more loose stools per day for two or more days), often accompanied by cramping, fever, and sometimes blood. It doesn’t improve with over-the-counter remedies and gets worse without treatment.

vanessa k
November 14, 2025 AT 06:36My uncle got C. diff after one clindamycin pill for a tooth abscess. He was in the ICU for three weeks. They had to remove part of his colon. Don't let anyone tell you it's 'just diarrhea.' This isn't a stomach bug-it's a silent killer that sneaks in after you think you're safe.
manish kumar
November 15, 2025 AT 01:00I read this entire thing twice because I'm a dentist in India and we prescribe clindamycin all the time for penicillin-allergic patients. I had no idea it was this dangerous. The stats about community cases-20% of all CDI-hit me hard. I'm changing my protocol tomorrow. I'm going to start asking patients if they've had any gut issues in the past, and I'm going to give them a printed sheet with the symptoms to watch for. We can't keep treating antibiotics like candy. This isn't just about one drug-it's about how we think about the microbiome. Your gut isn't just a pipe-it's a whole ecosystem, and we're nuking it with broad-spectrum drugs like it's a bug spray.
Nicole M
November 15, 2025 AT 18:23So if I took clindamycin for a wisdom tooth extraction six weeks ago and now I’ve had two loose stools today… should I just go to the ER or wait to see if it gets worse?
Arpita Shukla
November 16, 2025 AT 16:26You don't need to go to the ER for two loose stools. You need to get a stool test. And you need to stop taking probiotics because they're useless. The CDC doesn't recommend them. The only thing that works is vancomycin or fidaxomicin if it's confirmed. And no, loperamide is not your friend-it traps toxins. Also, hand sanitizer doesn't kill C. diff spores. Soap and water. Basic hygiene. You'd think this was common knowledge but apparently not.
Benjamin Stöffler
November 16, 2025 AT 19:44Clindamycin… a drug that, in its arrogance, believes it can selectively eradicate gram-positive flora… but in reality, it is a sledgehammer in a watchmaker’s workshop. It doesn’t ‘target’ bacteria-it annihilates. And in the vacuum it leaves behind, C. difficile, the ultimate opportunistic survivor, rises like a phoenix from the ashes of your gut microbiome. You think you’re treating an abscess? No-you’re surrendering your intestinal sovereignty to a spore that’s been waiting for millennia to exploit your modern ignorance. The FDA warning? Too little. Too late. This isn’t a side effect-it’s a systemic betrayal by pharmaceutical logic.
Mark Rutkowski
November 18, 2025 AT 07:24It’s wild how we treat antibiotics like magic bullets-pop one, feel better, forget it. But your gut? It’s not a broken pipe you fix and move on. It’s a rainforest. And clindamycin doesn’t just cut down a few trees-it burns the whole thing down and calls it ‘treatment.’ The real tragedy? We’re not just risking our own health-we’re handing the next person a spore on the bathroom door handle. We’re all connected in this invisible web. Maybe the real cure isn’t a drug-it’s humility. Ask the question: ‘Do I really need this?’ Before you swallow that pill, pause. Breathe. Your microbiome is counting on you.
Ryan Everhart
November 18, 2025 AT 08:21So let me get this straight-you’re telling me I can take one pill, feel fine, and then get a life-threatening infection 11 weeks later… and the only way to know is to monitor my poop? And if I don’t? I die? Cool. Thanks for the heads up. I’ll add ‘poop journaling’ to my daily routine right after yoga and before my 7 a.m. coffee. /s
David Barry
November 18, 2025 AT 23:45Let’s be real-this post is 90% fearmongering. The absolute risk of CDI from clindamycin is 1-2%. That’s less than getting hit by lightning. You’re more likely to die from a fall in the shower. The real issue? Overdiagnosis. Too many doctors order stool tests for mild diarrhea and turn normal gut fluctuations into ‘C. diff.’ That’s how you create a false epidemic. Stop panicking. Stop testing. Stop treating every loose stool like it’s the end of the world.