Bone Health Screening: Understanding DEXA Scan Results and Fracture Risk
 Nov, 9 2025
Nov, 9 2025
What a DEXA Scan Actually Measures
You’ve been told you need a DEXA scan. Maybe your doctor mentioned osteoporosis risk, or you’re over 65 and your insurance covers it. But what does this scan actually show? It’s not just a picture of your bones. A DEXA scan measures bone mineral density - how much calcium and other minerals are packed into a given area of your bone. This number tells your doctor how strong your bones are right now, and how likely you are to break one in the next few years.
The scan uses two very low-dose X-ray beams - one high energy, one low - passed through your hip and spine. The machine calculates how much of each beam gets absorbed by your bone versus soft tissue. The result? A number in grams per square centimeter. It’s simple, quick (usually under 15 minutes), and exposes you to less radiation than a day of normal sunlight.
Unlike CT scans or MRIs, DEXA doesn’t show structure or shape. It doesn’t tell you if a bone is cracked. It tells you how dense it is. And that’s the key to predicting fracture risk.
Understanding Your T-Score: The Most Important Number
Your DEXA report will give you a T-score. This is the number that matters most. It compares your bone density to the average peak bone mass of a healthy 30-year-old adult of the same sex and race.
- T-score of -1.0 or higher: Normal bone density. Your bones are in good shape.
- T-score between -1.0 and -2.5: Osteopenia. Your bone density is lower than normal, but not low enough to be called osteoporosis. This is a warning sign.
- T-score of -2.5 or lower: Osteoporosis. Your bones are significantly weaker. Fracture risk rises sharply here.
For example, a T-score of -2.7 means your bone density is 2.7 standard deviations below the young adult average. That’s not just a little low - it’s in the osteoporosis range. The lower the number, the higher your risk of breaking a bone.
Many people panic when they see a T-score of -1.8. But osteopenia doesn’t mean you’ll break a bone tomorrow. It means you need to pay attention. Lifestyle changes can slow or even reverse the loss.
Why Z-Scores Matter (And When They Don’t)
Not everyone compares to a 30-year-old. If you’re under 50, pregnant, or have a condition like rheumatoid arthritis, your doctor might look at your Z-score instead. This compares your bone density to people your own age, sex, and size.
A Z-score below -2.0 in a younger person is unusual. It suggests something else might be going on - like a hormone problem, malabsorption, or long-term steroid use. In those cases, your doctor will dig deeper.
But for most people over 50, the Z-score is just background noise. The T-score is what guides treatment. Don’t get distracted by the Z-score unless your doctor tells you to.
Fracture Risk Isn’t Just About Bone Density
Here’s the catch: a low T-score doesn’t always mean you’ll break a bone. And some people with normal bone density still fracture. Why? Because bone strength isn’t just about density. It’s about structure, quality, and your body’s ability to stay upright.
This is where FRAX comes in. Developed by the World Health Organization, FRAX is a free online tool that combines your T-score with other risk factors:
- Age
- Sex
- Weight and height
- History of previous fractures
- Family history of hip fracture
- Smoking
- Alcohol use (3+ drinks per day)
- Use of steroid medications
- Rheumatoid arthritis
FRAX calculates your 10-year risk of a major osteoporotic fracture (hip, spine, forearm, shoulder) and your risk of a hip fracture specifically. If your risk is above 20% for a major fracture or 3% for a hip fracture, most doctors will recommend treatment - even if your T-score is only in the osteopenia range.
One real case: a 70-year-old woman with a T-score of -2.1 (osteopenia) had a previous wrist fracture at 65. Her FRAX score put her 10-year hip fracture risk at 6.8%. She started a bone-strengthening medication and avoided a hip fracture two years later. Her T-score alone wouldn’t have triggered treatment. FRAX did.
What DEXA Can’t Tell You
DEXA is powerful, but it has blind spots.
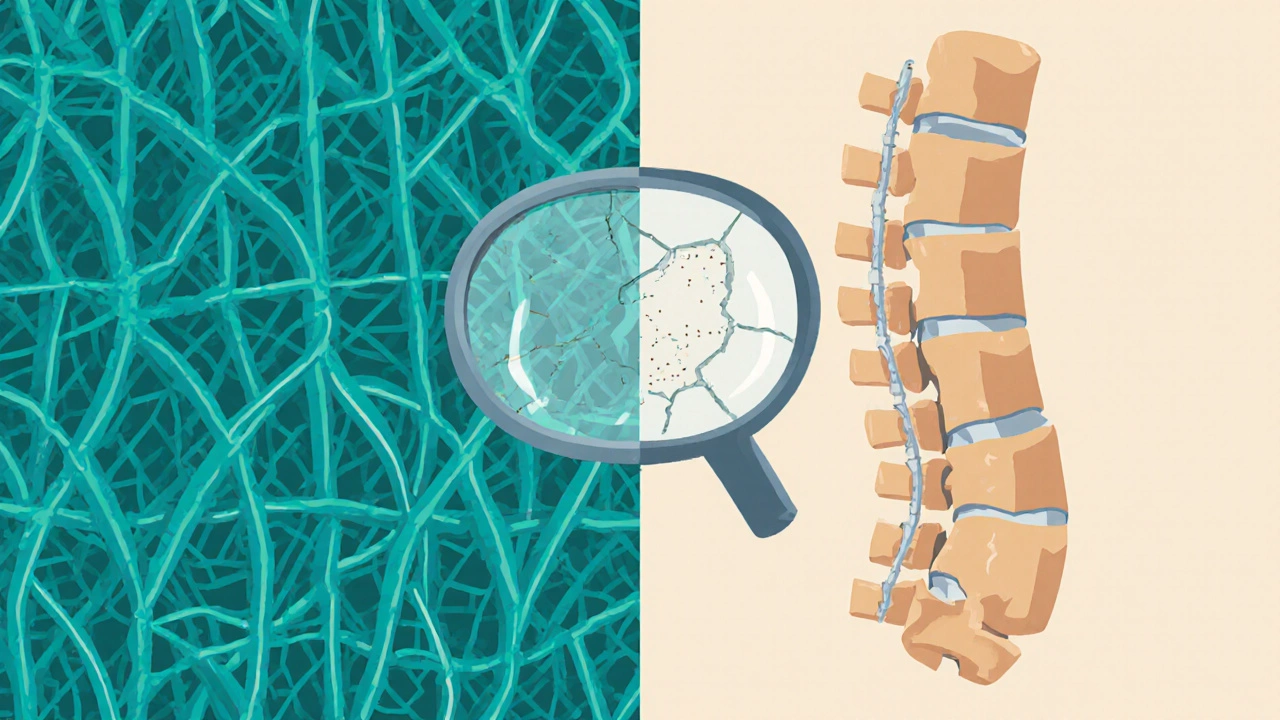
It can’t tell the difference between cortical bone (the hard outer shell) and trabecular bone (the spongy inner network). That matters because osteoporosis often starts in trabecular bone - the kind in your spine and hip. A normal DEXA result doesn’t guarantee your inner bone structure is healthy.
It also struggles with people who have severe arthritis, spinal fusion, or aortic calcification. Calcium deposits in arteries can look like bone on the scan, making your T-score falsely high. That’s why your technologist needs to know your full medical history.
And DEXA doesn’t measure bone quality - how well your bone tissue is connected, how much microdamage has built up, or how flexible your bones are. That’s where newer tools like Trabecular Bone Score (TBS) are starting to help. TBS analyzes the texture of your spine image from the DEXA scan to estimate bone structure. Studies show it improves fracture prediction by up to 18% when added to T-score.
Who Should Get a DEXA Scan?
Not everyone needs one. But if you fit any of these criteria, screening is strongly recommended:
- Women 65 or older
- Men 70 or older
- Postmenopausal women under 65 with risk factors (low body weight, smoking, steroid use, family history)
- Men 50-69 with risk factors
- Anyone who broke a bone after age 50 from a minor fall
- Anyone taking long-term steroid medication (like prednisone for 3+ months)
- People with conditions linked to bone loss: rheumatoid arthritis, hyperthyroidism, celiac disease, chronic kidney disease
Medicare covers DEXA every two years for eligible people. Most private insurers follow the same rules. If you’re unsure, ask your doctor - or call your insurance. Don’t assume you don’t qualify.
What Happens After Your Scan?
Getting your results is just the start. What you do next determines your risk.
If your T-score is normal: Keep doing what you’re doing. Get enough calcium (1,200 mg/day), vitamin D (800-1,000 IU/day), and weight-bearing exercise (walking, dancing, lifting weights). Avoid smoking and limit alcohol.
If you have osteopenia: Talk to your doctor about lifestyle changes first. Many people can stabilize or even improve their bone density with diet, exercise, and fall prevention. But if your FRAX score is high, or you’ve already had a fracture, medication may be needed.
If you have osteoporosis: Medication is usually recommended. Options include bisphosphonates (like alendronate), denosumab, teriparatide, or romosozumab. These aren’t magic pills - they reduce fracture risk by 30-70% depending on the drug and site. But they work best when combined with lifestyle changes.
Follow-up scans are typically done every 1-2 years if you’re on treatment. More often if you’re at high risk. Less often if your bone density is stable and you’re not on meds.
Common Misconceptions and Patient Fears
Many people avoid DEXA scans because they’re scared of radiation. The truth? One scan equals less than two days of natural background radiation. You get more from a cross-country flight. The benefit far outweighs the tiny risk.
Others think a low T-score means they’re doomed. But osteoporosis is treatable. Many people live for years without fractures after starting treatment.
And yes, insurance can be a hassle. About 32% of patients report coverage issues. If your claim is denied, ask your doctor to write a letter of medical necessity. Many denials are overturned on appeal.
What’s Next for Bone Health Screening?
The field is evolving. AI tools are now being trained to spot hidden spine fractures on DEXA scans - something even experienced radiologists sometimes miss. One 2023 study showed AI detected 94.7% of vertebral fractures automatically.
Portable DEXA devices are becoming more common in pharmacies and clinics, making screening easier in rural or underserved areas. And researchers are exploring blood tests that might one day predict bone loss before it shows up on a scan.
But for now, DEXA remains the gold standard. No other test has been proven as reliable in predicting who will break a bone. If you’re at risk, don’t wait. Get screened. Know your number. Take action.

Lashonda Rene
November 10, 2025 AT 09:30i just got my dexa results and honestly i was scared outta my mind like my bones are gonna turn to dust or something?? but then i read that a t-score of -1.8 is just osteopenia and not osteoporosis and i was like... wait, that’s not a death sentence?? i’ve been walking my dog every morning and eating yogurt like it’s my job and i think that helped. also i stopped drinking soda. who knew? maybe my bones are just tired of sugar and caffeine. anyway, don’t panic. your body’s smarter than you think.
Clyde Verdin Jr
November 10, 2025 AT 14:34lol this whole post is just pharma marketing dressed up as medicine 😂
DEXA scans are basically glorified scales that measure calcium like it’s the only thing that matters. ever heard of collagen? or bone elasticity? nah, they don’t teach that in med school because it doesn’t sell drugs. and FRAX? more like FRAX-UP-fraudulent risk algorithm eXaggeration. my uncle had a t-score of -3.2 and rode a motorcycle until he was 82. he didn’t need bisphosphonates, he needed a better sense of humor. 💀
Key Davis
November 11, 2025 AT 20:02Thank you for this comprehensive and clinically accurate overview. The distinction between T-scores and Z-scores is frequently misunderstood by patients, and your clarification regarding FRAX is particularly valuable. I encourage all clinicians to share this resource with their patients, as informed decision-making is foundational to effective osteoporosis management. The inclusion of real-world case examples enhances both accessibility and credibility. Well done.
Cris Ceceris
November 12, 2025 AT 15:21it’s wild how we treat bones like a bank account-deposit calcium, withdraw strength, check the balance once a year and panic if it’s low. but bones aren’t just mineral deposits, right? they’re alive. they remodel, they adapt. maybe the real question isn’t ‘how dense are they?’ but ‘how alive are they?’
why do we ignore the blood flow, the nerve signals, the mechanical stress from daily movement? i think we’re scared of complexity. easier to give a number and a pill than to ask someone to move differently, eat differently, live differently.
is it possible that our fear of falling is what’s actually breaking us?
Brad Seymour
November 13, 2025 AT 01:40man i love this post. finally someone explains it without jargon. i’m from the uk and we get these scans free on the nhs but half my mates think it’s a scam. i told my mum she needs one after she dropped a kettle on her foot and broke her toe. she said ‘it’s just a toe!’ i said ‘no, it’s a warning.’ she got scanned, t-score -2.0, started vitamin d and now she’s doing tai chi with a group of 70-year-olds who all call each other ‘grandma warrior.’ it’s beautiful. 💪❤️
Malia Blom
November 13, 2025 AT 21:59ok but what if the ‘normal’ 30-year-old they’re comparing you to was on steroids and drank protein shakes all day? what if they never walked more than 200 feet? why are we measuring against some mythical peak that only exists in pharmaceutical brochures?
also, why is osteopenia even a diagnosis? it sounds like a word made up to sell supplements. ‘oh honey, your bones are... osteopenic. here’s a $120 bottle of calcium gummies.’
also, why do we assume everyone wants to live to 90? maybe i just wanna die skiing at 75. not all of us are scared of death. some of us are scared of being bored.
Erika Puhan
November 15, 2025 AT 03:15the entire premise of DEXA screening is statistically flawed. population-based norms are culturally and genetically homogenized, ignoring epigenetic variation in bone metabolism across ethnicities. the T-score paradigm is rooted in a eurocentric, young-adult reference cohort that fails to account for ancestral bone density adaptations-particularly in populations with high physical activity load and low dairy intake. furthermore, the overreliance on FRAX neglects biomechanical loading history, which is a stronger predictor than mineral density alone. this is medical reductionism at its finest. 🤦♀️
Edward Weaver
November 15, 2025 AT 13:09they let anyone get a dexa scan now? next they’ll be scanning your kidneys for ‘low kidney density’ and selling you kidney pills. this is why america’s healthcare is broke. you’re telling me a 65-year-old woman needs a scan just because she’s old? what’s next? ‘hey ma’am, your spleen is 12% below average for your age, here’s a $500 treatment plan.’
we used to just walk, eat food, and not die of fear. now we’re all walking around scared of our own skeletons. get off the couch, lift something heavy, and stop letting corporations turn your bones into a product.
Lexi Brinkley
November 17, 2025 AT 07:37my grandma got her dexa scan and the doc said she had osteoporosis 😭
she said ‘so i’m just a walking ghost now?’
we started her on walking, eggs, and sunshine. now she’s doing yoga with her grandkids and posting memes about ‘bone boss energy’ 💪🦴
she’s 78. she’s not broken. she’s upgraded. 🌞✨
Kelsey Veg
November 18, 2025 AT 05:04my t-score was -2.5 and i cried for 3 days. then i found out my mom had the same score and she’s 81 and still hikes. so i stopped crying and started lifting dumbbells. now i do 10lbs every morning. my bones aren’t perfect, but they’re mine. and i’m not letting some machine tell me i’m weak.