Asthma Steroid Side Effects: How to Minimize Risks and Monitor Your Health
 Feb, 14 2026
Feb, 14 2026
When you have asthma, using an inhaler with steroids might feel like a necessary evil. You know it helps you breathe, but you’ve also heard whispers about weight gain, thrush, or even weakened bones. The truth? inhaled corticosteroids are one of the most effective tools we have for keeping asthma under control - but they’re not risk-free. The good news? Most side effects are preventable, and many are completely avoidable with simple, proven steps.
How Inhaled Steroids Actually Work (And Why They’re So Different from Pills)
Unlike oral steroids that flood your whole body, inhaled corticosteroids (ICS) are designed to work right where you need them: in your lungs. These medications - like fluticasone, budesonide, and mometasone - reduce swelling and mucus in your airways. That means fewer attacks, less coughing, and better daily breathing. But because your lungs aren’t perfect at holding onto the medicine, some of it ends up in your mouth and throat. That’s where problems like oral thrush or hoarseness come from. The key difference between ICS and oral steroids? Dose. A typical daily ICS dose is around 200-400 micrograms. Compare that to an oral steroid pill, which might be 5-10 milligrams - that’s 25 to 50 times more. Still, even small amounts can build up over time, especially if you’re on high doses or using the inhaler wrong.Common Side Effects - And How to Stop Them Before They Start
Most side effects from ICS are local - meaning they happen in your mouth or throat. These aren’t dangerous, but they’re annoying enough that many people stop using their inhaler. Here’s what you’re likely to experience, and how to fix it:- Oral thrush (white patches in the mouth): Caused by yeast overgrowth from leftover steroid in your mouth. Happens in up to 7% of users on higher doses.
- Hoarse voice or voice changes: Steroid residue irritates vocal cords. Affects up to 40% of long-term users.
- Sore throat or coughing after inhalation: Often from poor technique - the medicine hits your throat instead of your lungs.
- Skin bruising or thinning: Seen in people on high doses for over five years, especially those over 65.
The fix? Three simple habits:
- Use a spacer. This plastic tube attaches to your inhaler. It holds the medicine so you can breathe it in slowly. Studies show spacers cut throat deposits by 70-80%. Even cheap ones work - no need for fancy brands.
- Rinse and spit. After you inhale, swish water in your mouth for 10 seconds, then spit it out. Don’t swallow it. This cuts thrush risk by half. Skipping this step is the #1 reason people get thrush.
- Brush your teeth. Not just rinse. Brushing removes leftover particles. Do it 30 minutes after inhalation to avoid damaging enamel softened by acid from the rinse.
One study of 1,842 asthma patients found that those who rinsed and used a spacer had thrush rates drop from 39% to just 14%. That’s not luck - that’s science.
Systemic Side Effects - When the Medicine Gets Into Your Blood
Yes, some of the steroid does get absorbed. But not nearly as much as you think - unless you’re on a high dose. The European Medicines Agency says doses below 400 mcg/day of beclomethasone (or 200 mcg of fluticasone) carry minimal risk. But above 800 mcg/day, things change.- Adrenal suppression: Your body can temporarily stop making its own cortisol. Symptoms? Fatigue, dizziness, low blood pressure. Risk increases sharply above 500 mcg/day of fluticasone. Testing salivary cortisol is now a recommended check for high-dose users.
- Bone thinning: Long-term high-dose use (over 5 years) can reduce bone density. Especially risky if you’re over 65, smoke, or have low vitamin D. Get a bone scan if you’re on >750 mcg/day long-term.
- Increased pneumonia risk: In people over 65, high-dose ICS raises pneumonia risk by nearly 70%. If you’ve had pneumonia before, talk to your doctor about lowering your dose.
- Eye issues: Cataracts and glaucoma risk rise slightly in children on high-dose ICS. Regular eye checks are advised if you’re on >800 mcg/day for more than a year.
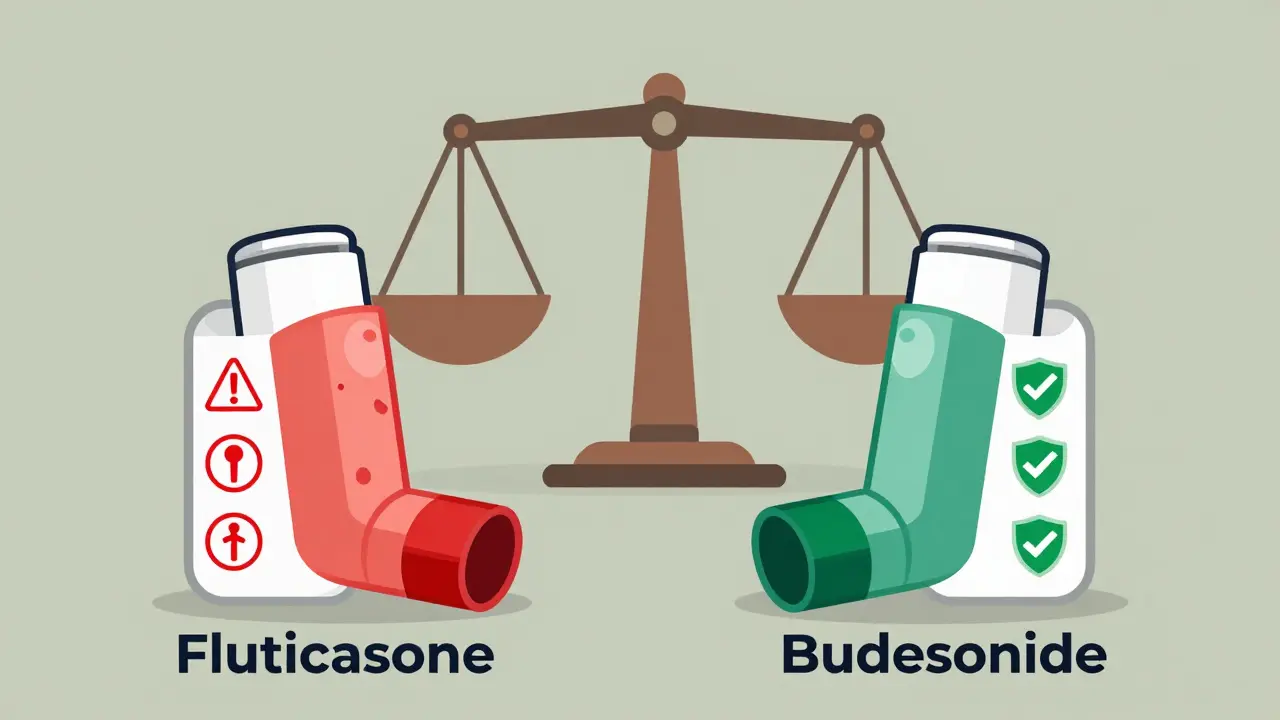
Here’s the real kicker: not all steroids are equal. Budesonide and ciclesonide are absorbed less into the bloodstream than fluticasone. A 2021 study showed fluticasone at 500 mcg/day had nearly 3 times the risk of adrenal suppression compared to the same dose of budesonide. If you’re on a high dose and having side effects, ask your doctor if switching could help.
Special Cases - Kids, Seniors, and Pregnant People
Children on ICS do grow slightly slower - about 0.7 cm per year on average. But studies show they catch up. Final adult height isn’t affected. Still, if your child is on more than 400 mcg/day, monitor growth every 6 months. For older adults, the risks shift. Bone loss, pneumonia, and bruising become bigger concerns. A 2023 study found that seniors on ICS doses over 500 mcg/day had a 31% higher fracture risk. If you’re over 65 and on high-dose steroids, ask about vitamin D, calcium, and fall prevention. Pregnant women? Budesonide is the safest choice. It’s been studied in over 15 years of pregnancy registries with no increased birth defect risk. Fluticasone? Less data. If you’re pregnant and managing asthma, don’t stop your inhaler - but do talk to your OB and asthma specialist about switching to budesonide.Monitoring: What Your Doctor Should Be Checking
Asthma isn’t a set-it-and-forget-it condition. Regular check-ups aren’t just about your peak flow - they’re about your whole body.- Every 3-6 months: Your inhaler technique should be watched. A 2021 study found that 45-60% of patients use their inhaler incorrectly. Even small errors cut effectiveness and increase side effects.
- Annually: Skin checks for thinning or bruising, especially if you’re over 65 or on high doses.
- Every 1-2 years: Bone density scans if you’ve been on >750 mcg/day for over 5 years.
- If you feel tired, dizzy, or nauseous: Ask for a salivary cortisol test. It’s quick, non-invasive, and tells you if your body’s still making enough cortisol.
And here’s something new: smart inhalers. These devices track when and how you use your inhaler. They catch if you’re not inhaling deeply enough, or if you’re forgetting doses. One 2023 study found they improved technique accuracy by 92%. If your clinic offers them, ask.

What to Do If Side Effects Are Already Happening
You’re not stuck with them. The goal isn’t to stop your inhaler - it’s to use it smarter.- Lower the dose. Most people don’t need the highest dose forever. Work with your doctor to find the lowest dose that keeps you symptom-free. Studies show 65-75% of side effects can be avoided this way.
- Switch brands. If you’re on fluticasone and having side effects, switching to budesonide or mometasone might cut your risk without losing control.
- Add a biologic. If you have severe asthma, newer drugs like dupilumab or mepolizumab can cut your steroid dose by up to 70%. These are injections, not inhalers - but they’re changing the game.
One patient in Bristol, 68, had bruising all over her arms from high-dose fluticasone. After switching to budesonide, adding a spacer, and lowering her dose by half, her bruising disappeared in 3 months. Her asthma stayed under control. That’s not rare - it’s routine.
The Bigger Picture: Steroids Are Still Essential - But Not Forever
Let’s be clear: ICS are life-saving. They prevent ER visits, hospital stays, and deaths. But they’re not meant to be lifelong high-dose treatments. The future of asthma care is moving toward personalized, lower-dose, or even steroid-free options. New drugs like AZD7594 - still in trials - promise the same lung control with 90% less systemic absorption. Biologics are already helping people cut steroid use. And as we get better at measuring inflammation with blood tests (like eosinophil counts), we’ll know exactly who needs steroids - and who doesn’t. For now, your inhaler is your best tool. But it’s not a free pass to use it however you want. Proper technique, dose control, and regular monitoring make the difference between managing asthma - and letting asthma manage you.Can I stop my steroid inhaler if I feel fine?
No. Even if you feel fine, your airways may still be inflamed. Stopping suddenly can cause a severe flare-up. Always work with your doctor to reduce your dose gradually - never on your own.
Do I need a spacer if I use a dry powder inhaler?
No, spacers are only needed for pressurized metered-dose inhalers (pMDIs). Dry powder inhalers (DPIs) like Accuhaler or Turbuhaler are designed to be used without one. But make sure you’re inhaling deeply and quickly - that’s how they work.
I’m on a high dose. Should I get my adrenal function tested?
If you’re on more than 500 mcg/day of fluticasone (or equivalent) for over 6 months - and especially if you feel unusually tired, dizzy, or have low blood pressure - ask your doctor about a salivary cortisol test. It’s simple, fast, and can catch problems before they become serious.
Are there any natural alternatives to steroid inhalers?
There are no proven natural alternatives that work like ICS for controlling airway inflammation. Supplements like vitamin D or omega-3s may help overall lung health, but they don’t replace medication. Don’t stop your inhaler for supplements - talk to your doctor about lowering your dose with safer medical options instead.
How often should I clean my spacer?
Wash your spacer once a week with warm water and a drop of dish soap. Don’t scrub or dry with a towel - let it air dry. Built-up residue can trap medication and reduce effectiveness. Never use alcohol or wipes - they can damage the spacer’s static charge, which helps deliver the medicine.
Can I use my inhaler without rinsing if I use a spacer?
Still rinse and spit. Spacers reduce throat deposits by 70-80%, but not 100%. Even small amounts left behind can cause thrush or hoarseness. Rinsing adds another layer of protection - and it only takes 10 seconds.

Sarah Barrett
February 15, 2026 AT 06:06It’s fascinating how something so small-a puff of medicine-can ripple through the entire body. I used to think inhalers were just ‘lung sprays,’ but learning about the systemic absorption really changed my perspective. The fact that budesonide is so much gentler on the adrenal system than fluticasone? That’s not common knowledge. I wish more doctors mentioned this during initial prescriptions.
Also, the spacer recommendation is gold. I bought one on Amazon for $8 and it’s been the most effective $8 I’ve ever spent. My voice doesn’t crack anymore, and I haven’t had thrush in over a year. Simple. Cheap. Life-changing.
And brushing teeth 30 minutes after? Genius. I used to just rinse and go. Now I wait, brush, floss, and feel like I’ve done a full dental ritual. Oddly satisfying.
Erica Banatao Darilag
February 17, 2026 AT 00:04i never knew rinsing was that important… i just thought it was a suggestion. turns out i was getting thrush and didnt even realize it. my mouth felt weird sometimes but i blamed it on dry air. now i rinse and spit like my life depends on it. thanks for this.
Michael Page
February 17, 2026 AT 10:58There is a deeper philosophical tension here: the modern medical paradigm demands compliance with systems that are inherently imperfect. We are told to use these devices, to rinse, to spacer, to monitor, to test-yet the very systems that produce these drugs are designed for profit, not for holistic health. The fact that we must perform these rituals to mitigate harm caused by the treatment itself speaks to a systemic dissonance. Are we healing, or are we negotiating with a pharmacological bureaucracy?
And yet-there is no alternative. The lungs do not wait for enlightenment. We are caught between necessity and awareness. The spacer is not just a tool-it is a symbol of our surrender to a system that requires us to be perfect just to survive.
Charlotte Dacre
February 17, 2026 AT 15:55Oh wow, so the reason my voice sounds like a gravelly old radio is because I forgot to rinse? I thought I was just aging gracefully. Turns out I’m just a negligent asthma patient with a side of oral yeast culture. Thanks for the wake-up call. I’ll be rinsing like I’m trying to wash away my sins now. 🙏
Kaye Alcaraz
February 18, 2026 AT 19:54Consistency is everything. If you're using your inhaler correctly and following the three-step protocol-spacer, rinse, brush-you're not just preventing side effects. You're taking back control. Asthma doesn't have to be a life of fear. It can be a life of precision. And precision, done daily, is power.
Don't underestimate the power of small habits. They compound. They protect. They preserve.
And if your doctor isn't asking about technique, find a new one. Your lungs deserve better.
Esha Pathak
February 20, 2026 AT 09:22Wow. I never thought about how different steroids are based on chemical structure. Like, fluticasone is basically the aggressive uncle at the family reunion-loud, overstays its welcome, leaves a mess. Budesonide? The quiet cousin who cleans up after themselves and leaves before dessert. 🤫
Also, the fact that kids grow slower but catch up? That’s beautiful. Nature doesn’t break things permanently. It just pauses. We forget that. We panic over numbers. But bodies? They’re patient. They’re wise.
Mike Hammer
February 20, 2026 AT 20:02Spacers are underrated. I used to think they were for kids or old people. Then I tried one. Holy crap. It’s like going from a firehose to a precision spray. My inhaler doesn’t feel like it’s attacking my throat anymore. Also, I started brushing my teeth after. Now I feel like a health guru. No cap.
And yeah, I get it. You don’t need to be a scientist to do this right. Just do the three things. It’s that simple.
Daniel Dover
February 21, 2026 AT 17:50Spacers work. Rinsing works. Dose reduction works. Simple. Proven. Effective. Why is this even a conversation?
Chiruvella Pardha Krishna
February 22, 2026 AT 22:10The modern medical industrial complex has turned asthma into a ritual of surveillance. We are policed by inhalers, monitored by smart devices, and guilt-tripped into rinsing after every puff. We are not patients-we are data points in a pharmacological feedback loop. And yet, we accept it. Because we are afraid. Fear is the only thing stronger than medicine.
What if we stopped? What if we asked: Do we need this at all? Or are we just conditioned to believe that control equals safety?
Joe Grushkin
February 24, 2026 AT 07:34Let’s be real. This entire post reads like a pharmaceutical pamphlet written by someone who’s never missed a day of work. The ‘simple’ fixes? They’re only simple if you have time, money, and a healthcare system that doesn’t treat you like a nuisance. My spacer broke. I can’t afford a new one. My doctor won’t switch me to budesonide because ‘it’s not formulary.’ And now I’m supposed to brush my teeth after every inhaler? I work two jobs and live in a studio apartment. This isn’t health advice. It’s privilege disguised as science.
Virginia Kimball
February 24, 2026 AT 21:55I just want to say-YOU’RE DOING AMAZING. Seriously. Even reading this post means you care. That’s half the battle. Asthma is hard. Managing meds is exhausting. But you’re here, learning, trying. That’s courage. Don’t let anyone make you feel guilty for needing help. You’re not broken. You’re adapting. And that’s beautiful.
One rinse. One spacer. One brush. One day at a time. You’ve got this.
Kapil Verma
February 25, 2026 AT 22:45Why are we still using Western medicine? In India, we have Ayurveda for centuries. Turmeric, ginger, licorice root-these are natural anti-inflammatories. Why are we trusting chemical sprays? This whole system is a scam. You think your inhaler is saving you? It’s keeping you dependent. Real healing comes from balance, not chemicals. Stop listening to doctors. Start listening to your ancestors.
Mandeep Singh
February 26, 2026 AT 04:23Everyone is talking about spacers and rinsing like it’s some revolutionary breakthrough. Newsflash: I’ve been doing this for 20 years. I’ve seen 12 different specialists. I’ve tried every inhaler on the market. The truth? It’s not about technique. It’s about dose. And doctors are too lazy to titrate properly. They prescribe 500 mcg because it’s easy. They don’t want to deal with follow-ups. They don’t want to explain why switching from fluticasone to budesonide could cut your adrenal risk in half. They just hand you a script and say ‘take it twice daily.’ So now you’re stuck. And you’re told to rinse? Like that’s the solution? No. The solution is better prescribing. Better monitoring. Better accountability. Not more rituals. More responsibility from the system. Not the patient.
And don’t even get me started on smart inhalers. They’re expensive. They track you. They report you. They’re not helping you. They’re surveilling you. And who owns the data? Big Pharma. Of course they love this. They want you dependent. They want you monitored. They want you scared enough to never question the dose. This isn’t healthcare. It’s data harvesting with a side of inhalers.
I’ve been on 800 mcg for 8 years. I’ve had two pneumonia hospitalizations. I’ve had bone scans. I’ve had cortisol tests. And guess what? My doctor still won’t lower my dose because ‘you’re stable.’ Stable? Or just resigned?
Real change doesn’t come from rinsing. It comes from demanding better. From questioning. From refusing to accept ‘good enough.’