Asthma and COPD Medications: Key Interactions and Safety Risks You Need to Know
 Jan, 9 2026
Jan, 9 2026
Asthma/COPD Medication Interaction Checker
This tool identifies potentially dangerous interactions between your respiratory medications and other common drugs. Based on clinical guidelines and FDA warnings.
Enter your medications to check for dangerous combinations. Based on FDA guidelines and clinical studies.
When you're managing asthma or COPD, your inhaler isn't the only thing that affects your breathing. Many of the pills, creams, and over-the-counter remedies you take every day can quietly interfere with your respiratory meds-sometimes with dangerous results. This isn't theoretical. Real people are ending up in hospitals because they didn't know that their painkiller, cold medicine, or even heart pill could make their lungs shut down.
What Medications Are You Really Taking?
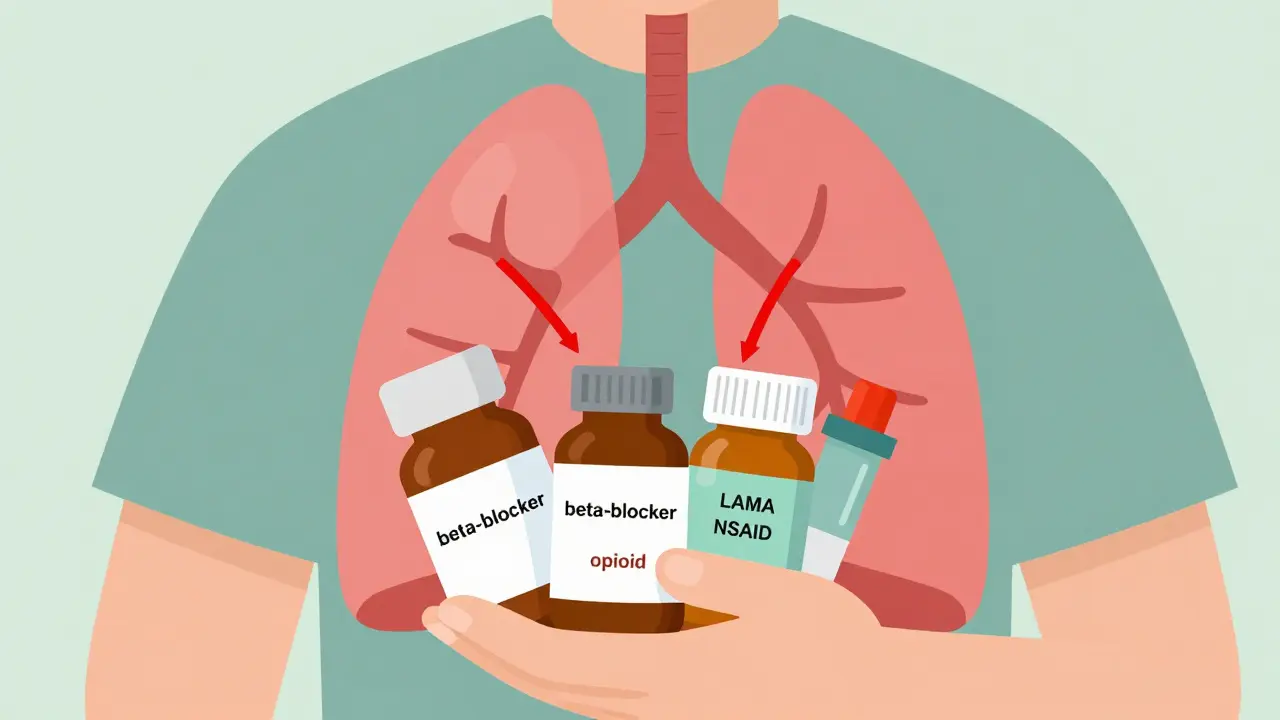
Most people with asthma or COPD are on multiple medications. That’s normal. But the more drugs you take, the higher the chance something will clash. Bronchodilators like albuterol, salmeterol, and tiotropium are the backbone of treatment. They open your airways. But they don’t work in isolation. Their effects can be canceled out-or made worse-by other drugs you might not even think of as lung-related.Take beta-blockers. These are commonly prescribed for high blood pressure, heart rhythm issues, or even anxiety. Nonselective ones like propranolol and nadolol block beta receptors everywhere-including in your lungs. For someone with asthma, that’s a red flag. Studies show these drugs can drop FEV1 (a key measure of lung function) by 15 to 25% in susceptible people. That’s not a small dip. That’s a potential emergency. Even if you’ve had asthma for years, a new heart medication could trigger your first severe attack.
Here’s the twist: selective beta-blockers like metoprolol are often safe for mild to moderate asthma. The 2021 BLOCK-COPD trial showed COPD patients on metoprolol had 14% fewer flare-ups than those on placebo. But you can’t guess. You need to talk to your doctor. Never start or stop a beta-blocker without checking.
The Hidden Danger: Opioids and Sedatives
If you’ve ever been prescribed oxycodone, hydrocodone, or codeine for pain, you need to pay attention. Opioids slow your breathing. That’s their job. But if your lungs are already struggling from COPD, that slowdown can become life-threatening.Combine opioids with benzodiazepines-like lorazepam or diazepam, often used for anxiety or sleep-and the risk of respiratory depression jumps by 300%. A 2022 FDA report found that 17% of opioid-related adverse events in COPD patients involved this combo. One Reddit user, COPDSurvivor87, described his oxygen levels dropping to 82% after mixing oxycodone with diphenhydramine (Benadryl). He ended up in the ER. That’s not rare.
Even antibiotics can be risky. Clarithromycin (Biaxin) and ketoconazole (Nizoral) interfere with how your body breaks down certain bronchodilators. This causes drug levels to build up in your blood, leading to tremors, rapid heartbeat, or worse. If you’re on a LABA like formoterol and your doctor prescribes one of these antibiotics, ask if there’s a safer alternative.
NSAIDs and Aspirin: The Silent Triggers
You take ibuprofen or naproxen for a headache. You assume it’s harmless. But for about 10% of adults with asthma-especially those with nasal polyps or chronic sinus issues-these common painkillers can trigger a severe bronchospasm within an hour.A user on r/asthma shared how a single dose of ibuprofen sent them into a full-blown attack. They didn’t know they were part of that 9-10% group. Asthma + Lung UK’s 2023 survey found that 31% of respondents had breathing problems linked to non-respiratory meds. Most didn’t connect the dots until it was too late.
Acetaminophen (paracetamol) is usually a safer choice for pain relief in asthma patients. But even that’s not foolproof. If you’re on corticosteroids long-term, your liver is already under stress. Mixing too much acetaminophen can add to that burden. Always check with your pharmacist before switching pain meds.
Anticholinergic Overload
LAMAs like tiotropium and glycopyrrolate are powerful tools for COPD. But they’re anticholinergics-meaning they block a nerve signal that tightens airways. The problem? So do many other drugs.Over-the-counter sleep aids like diphenhydramine (Benadryl), bladder meds like oxybutynin, tricyclic antidepressants like amitriptyline, and even some Parkinson’s drugs like benztropine all carry the same mechanism. When you stack them with your inhaler, you’re doubling down on anticholinergic effects.
That means dry mouth, constipation, blurry vision-and worse-urinary retention. The European Respiratory Society found a 28% spike in acute urinary retention among male COPD patients taking both LAMA inhalers and bladder meds. For older men, this isn’t just uncomfortable. It can lead to infections, kidney damage, or emergency catheterization.
There’s no need to stop your bladder medication. But you do need to tell your pulmonologist and pharmacist you’re on a LAMA. They can adjust the dose or switch you to a non-anticholinergic alternative like mirabegron.
What You Can Do Right Now
You don’t need to be a medical expert to protect yourself. Here’s what actually works:- Keep a real-time medication list. Write down every pill, inhaler, patch, cream, and supplement you take. Include dosages and why you take them. Update it every time you see a doctor.
- Do the brown bag test. Once a year, bring all your meds-yes, even the expired ones-in a bag to your appointment. Your doctor might not ask, but they’ll be glad you did.
- Ask your pharmacist. Pharmacists are trained to catch drug interactions. Don’t just pick up your prescription. Ask: “Could this affect my breathing?”
- Use the COPD Medication Safety App. Launched in 2023 by the COPD Foundation, this free app checks your meds against 95% of common drugs and flags risks in plain language.
- Know your warning signs. If you suddenly feel more short of breath, dizzy, or your heart races after starting a new medication, stop it and call your doctor. Don’t wait.
Why This Matters More Than Ever
The average COPD patient now takes 6-8 medications. Many are over 65. That means multiple specialists, multiple prescriptions, and multiple chances for something to go wrong. A 2022 study in the Journal of the American Pharmacists Association showed that when pharmacists actively reviewed COPD patients’ meds, dangerous combinations dropped by 43% in just 12 months.Electronic health records now have alerts for risky combos-but they’re not perfect. They miss over-the-counter drugs. They don’t always know about herbal supplements. That’s why your input matters.
The future of respiratory care isn’t just better inhalers. It’s smarter medication management. The FDA’s Sentinel Initiative and the European Medicines Agency are already pushing for stronger interaction warnings on labels. But you can’t wait for regulations to catch up. Your lungs are too important.
Final Thought: It’s Not About Fear. It’s About Control.
You didn’t choose to have asthma or COPD. But you can choose how you manage it. Most dangerous interactions aren’t caused by bad doctors or bad drugs. They’re caused by silence-by not asking, not checking, not speaking up.Take control. Know your meds. Talk to your team. Keep that list updated. Use the app. Ask the pharmacist. That’s how you breathe easier-not just today, but for years to come.
Can I take ibuprofen if I have asthma?
About 10% of adults with asthma, especially those with nasal polyps or chronic sinusitis, can have severe breathing reactions to ibuprofen and other NSAIDs. If you’ve ever had a breathing attack after taking a painkiller, avoid NSAIDs entirely. Use acetaminophen (paracetamol) instead-but always check with your doctor first, especially if you’re on long-term steroids.
Are beta-blockers safe for people with asthma?
Nonselective beta-blockers like propranolol are dangerous and should be avoided. They can cause severe bronchospasm. Selective beta-blockers like metoprolol are often safe for mild to moderate asthma, especially if you have heart disease. The BLOCK-COPD trial showed metoprolol actually reduced COPD flare-ups. But never start one without your doctor’s approval and monitoring.
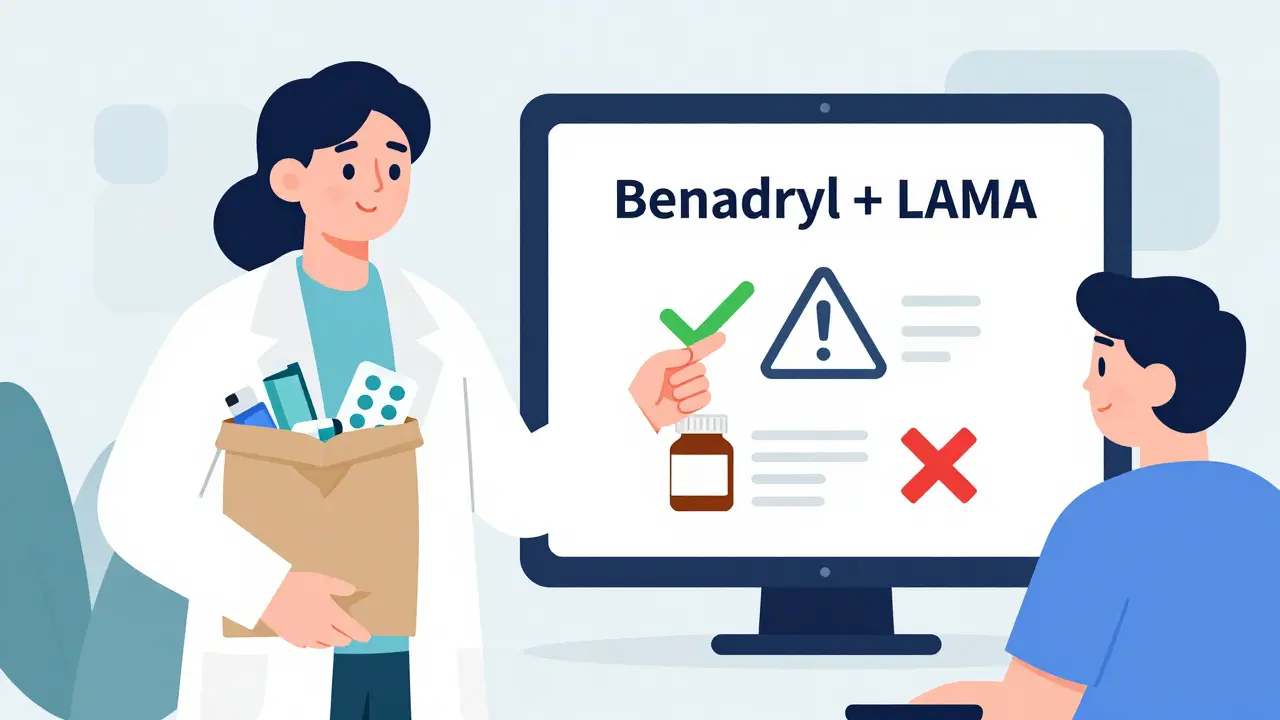
Can I use Benadryl if I’m on a LAMA inhaler?
Combining diphenhydramine (Benadryl) with a LAMA like tiotropium increases anticholinergic effects, raising the risk of dry mouth, constipation, urinary retention, and confusion-especially in older adults. Avoid OTC antihistamines unless your doctor says it’s okay. Try non-sedating options like loratadine instead.
What should I do if I’m on multiple medications for different conditions?
Create a complete, up-to-date list of every medication-including supplements and OTC drugs. Bring it to every appointment. Ask your pharmacist to review it for interactions. Use the COPD Medication Safety App to check new prescriptions before you take them. Polypharmacy is common, but dangerous combinations are preventable with vigilance.
How do I know if a new medication is affecting my breathing?
Watch for sudden changes: increased shortness of breath, wheezing, faster heart rate, dizziness, or trouble urinating. These can appear within hours of starting a new drug. If you notice them, stop the medication and contact your doctor immediately. Don’t wait for your next appointment. Your lungs can’t afford delays.

McCarthy Halverson
January 11, 2026 AT 04:34Keep the list. Talk to the pharmacist. Use the app. That's it.
Lisa Cozad
January 12, 2026 AT 23:54I used to ignore my OTC meds until I had a near-miss with ibuprofen. Now I check everything-even that ‘harmless’ sleep aid. My pulmonologist thanked me for bringing it up. Small things save lives.
Jay Amparo
January 14, 2026 AT 14:38As someone from India where polypharmacy is the norm, I’ve seen grandmas on 12 meds and zero coordination between doctors. This post? A lifeline. The COPD Safety App is now mandatory for my family. I showed my uncle how to use it-he cried because he didn’t know his bladder pill was making his breathing worse. We need more of this, not less.
Jake Nunez
January 16, 2026 AT 12:31My dad’s on metoprolol and tiotropium. His cardiologist didn’t mention the anticholinergic risk. His pharmacist did. Now he’s on mirabegron. Simple fix. Why don’t more doctors just ask what else you’re taking?
Saumya Roy Chaudhuri
January 17, 2026 AT 00:24Of course NSAIDs are dangerous for asthma-anyone with half a brain knows that. But the real issue is how lazy modern medicine has become. Doctors prescribe like it’s a buffet. You don’t need an app-you need a doctor who actually listens. And no, ‘just avoid ibuprofen’ isn’t enough. You need to know why.
Dwayne Dickson
January 18, 2026 AT 09:33While I appreciate the clinical rigor of this piece, I must emphasize that the systemic failure lies not in patient ignorance but in the fragmentation of care. The 2022 JAPhA study cited is corroborated by the 2023 Canadian Pharmacoepidemiology Review, which found that 68% of high-risk polypharmacy cases in COPD cohorts occurred when prescribers operated in silos without access to centralized medication reconciliation protocols. The FDA’s Sentinel Initiative, while commendable, remains under-resourced and reactive rather than proactive. Until interoperability between EHRs and community pharmacies becomes mandatory-not optional-we are merely rearranging deck chairs on the Titanic.
Jake Kelly
January 19, 2026 AT 05:34My mom’s on everything. She’s 72, has COPD, diabetes, and high BP. We do the brown bag thing every January. Last year we found three expired inhalers and a bottle of melatonin she didn’t even remember taking. We threw it all out. She’s breathing better. No magic, just attention.
Mario Bros
January 19, 2026 AT 14:31Benadryl + LAMA = bad news, folks 😬 I learned the hard way. Now I only use Zyrtec. Life’s better. No dry mouth, no urinary drama. Just breathe.
Bradford Beardall
January 21, 2026 AT 07:19Interesting how this mirrors what we see in geriatric care in rural Appalachia. Many elders take OTC meds because they’re ‘cheap’ or ‘free’-but no one tells them these interact. I’ve seen patients on tiotropium, oxybutynin, and amitriptyline-all prescribed by different docs. Their families don’t know to connect the dots. We need community health workers to do med reconciliation at senior centers. Not just apps.
Michael Marchio
January 22, 2026 AT 03:18Let’s be honest-most people don’t care until they’re gasping for air in the ER. I’ve reviewed over 300 COPD charts in my career. The pattern is always the same: someone starts a new painkiller, sleep aid, or beta-blocker, and suddenly they’re on a ventilator. The real tragedy isn’t the interaction-it’s that it was preventable. You didn’t die from asthma. You died because you didn’t ask the pharmacist. And that’s on you. Not your doctor. Not your meds. You.
Faith Edwards
January 22, 2026 AT 21:51How utterly pedestrian. This post reads like a pamphlet distributed at a Walgreens health fair. The real issue is the commodification of healthcare-where pharmaceutical conglomerates peddle synergistic toxicity as ‘convenience,’ and patients are conditioned to swallow anything labeled ‘OTC’ without a second thought. The fact that we need an app to prevent iatrogenic catastrophe speaks volumes about the moral bankruptcy of our system. If you’re still using diphenhydramine in 2024, you’re not just uninformed-you’re complicit in your own decline.
Christine Milne
January 23, 2026 AT 20:54Actually, in the U.S., we have the best medication safety infrastructure in the world. Other countries don’t even have electronic prescribing. You’re blaming the system, but the real problem is foreign patients who bring in unregulated supplements from India and China. I’ve seen cases where people take Ayurvedic pills with their inhalers and then blame American doctors. This isn’t about safety-it’s about cultural ignorance.