Antihypertensive Combination Generics: What’s Available and How to Get Them
 Jan, 5 2026
Jan, 5 2026
Most people with high blood pressure don’t need just one pill. They need two, sometimes three. But taking multiple pills every day? It’s easy to forget one. That’s where antihypertensive combination generics come in - single tablets that pack two or three blood pressure drugs into one. They’re not new, but their availability, cost, and insurance coverage still confuse patients and providers alike.
What Exactly Are Antihypertensive Combination Generics?
These are called Single-Pill Combinations (SPCs) or Fixed-Dose Combinations (FDCs). They combine two or more blood pressure medications into one tablet. Common pairings include:
- Amlodipine + benazepril (Lotrel)
- Losartan + hydrochlorothiazide (Hyzaar)
- Valsartan + amlodipine (Exforge)
- Amlodipine + valsartan + hydrochlorothiazide (Triamterene combo)
Each of these combinations targets blood pressure in different ways. One drug might relax blood vessels, another helps the body get rid of extra fluid, and a third blocks hormones that raise pressure. Together, they work better than either alone.
The FDA requires generic versions to match the brand-name drug’s performance within a strict range - 80% to 125% of the original in how the body absorbs it. That means if a brand-name pill lowers your pressure by 15 points, the generic should do the same. Studies back this up. In real-world use, these generics work just as well.
Why Do These Combinations Matter?
Almost 80% of people with high blood pressure need more than one medicine to reach their target. Yet, only about half of patients stick to their regimen. Why? Too many pills. Too many times to remember. Too many bottles to carry.
Switching to a single pill cuts the pill burden in half - or even more. Clinical trials show adherence jumps by 15% to 25% when patients move from multiple separate pills to one combination tablet. That’s not just convenience. It’s life-saving. Better adherence means fewer heart attacks, strokes, and hospital stays.
One patient on Reddit said: “Switched from three pills to one. My BP went from 158/94 to 122/82 in two months. I haven’t missed a dose since.” That’s not rare. It’s common.
What Combination Generics Are Actually Available?
As of 2023, over 30 different combination generics are on the market in the U.S. and globally. Here’s what you can realistically find:
| Combination | Generic Brand | Typical Dose | Monthly Cost (Cash Price) |
|---|---|---|---|
| Amlodipine + Benazepril | Lotrel | 5mg/20mg | $17.55 |
| Losartan + Hydrochlorothiazide | Hyzaar | 50mg/12.5mg | $10.60 |
| Amlodipine + Valsartan | Exforge | 5mg/160mg | $18.75 |
| Benazepril + Hydrochlorothiazide | Lotensin HCT | 10mg/12.5mg | $38.05 |
| Amlodipine + Valsartan + HCTZ | Triamterene combo | 5mg/160mg/12.5mg | $42.10 |
These prices are for cash-paying customers using GoodRx coupons. Insurance prices vary wildly - sometimes worse, sometimes better. But even at these rates, many combinations cost less than buying the individual drugs separately.
But here’s the twist: sometimes, buying the pills separately is cheaper. If you’re on generic amlodipine ($4.50/month) and generic valsartan ($7.80/month), that’s $12.30 total. The combo pill? $18.75. So why take the combo? Because it’s one pill. One routine. One less thing to forget.
When Does the Combo Pill Make Sense?
It’s not always the best choice. Here’s when it works:
- You’re just starting treatment and your doctor expects you’ll need two drugs.
- You’re already taking two separate pills and struggling to remember them.
- Your insurance covers the combo pill better than the individual ones.
- You’re on a fixed income and want to reduce pharmacy trips.
It’s less ideal when:
- You need fine-tuned dosing - like 2.5mg of amlodipine with 160mg of valsartan. That combo doesn’t exist as a pill.
- Your insurance charges you more for the combo than the two generics separately.
- You’re sensitive to one ingredient and need to adjust doses independently.
Doctors often start patients on a combo pill if their blood pressure is over 140/90. The 2018 STRIP trial showed 68% of patients hit their target with a combo pill versus only 45% with one drug at a time. That’s a big difference.

Insurance Gotchas - The Hidden Trap
This is where things get messy. Many patients assume if the pills are generic, insurance will cover the combo just like the individual ones. That’s not true.
On PatientsLikeMe, one user wrote: “My insurance covers each generic for $5. The combo? $45. It’s the same drugs. Why?”
Insurance companies often treat combination pills as “brand-like” even when they’re generic. They’ll cover the two separate pills at $5 each but charge $40+ for the single pill. Why? Because they don’t get a rebate from the manufacturer on the combo - or they’re trying to push patients toward cheaper, separate generics.
Always check your plan’s formulary. Call your insurer. Ask: “If I get the two separate generics, what’s my copay? What’s the copay for the combination?” Don’t assume. It can cost you hundreds a year.
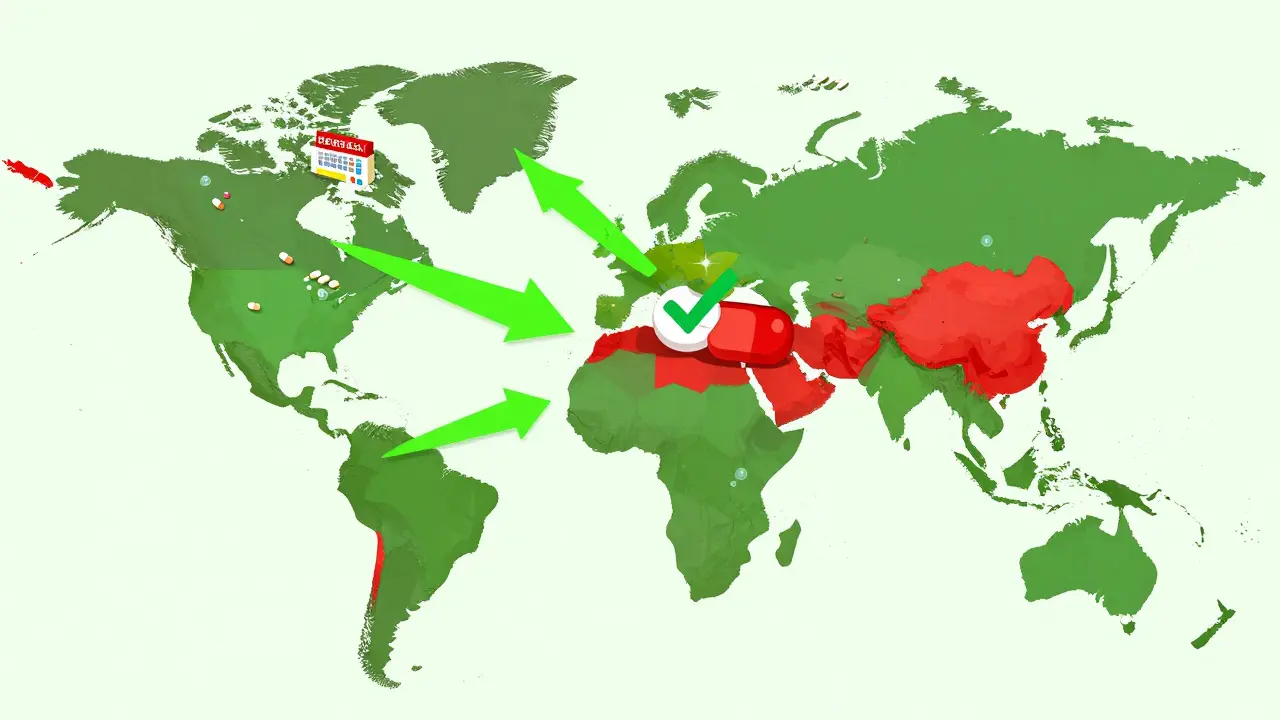
Global Availability - The Big Picture
In the U.S., 85% of antihypertensive prescriptions are for generics - and most of those are combinations. But globally? It’s a different story.
In low-income countries, only 15% of patients have access to combination generics - even though 95% of them need them. The WHO reports that in 46% of low-income countries, essential antihypertensive medicines - including combos - are available in fewer than half of pharmacies.
Why? Manufacturing, distribution, and pricing barriers. A pill that costs $10 in the U.S. might cost $20 or more in Nigeria or Bangladesh. Even when available, doctors often don’t know about them. Only 12 of 26 countries surveyed had SPCs in their national guidelines.
This isn’t just a U.S. problem. It’s a global health crisis. Only 7% of hypertension patients in low-income countries control their blood pressure. In high-income countries? Over 50%. Access to combination pills is one of the biggest reasons why.
What’s Changing in 2026?
The FDA released new draft guidance in late 2023 to make it easier to approve new generic combinations. That means more options are coming - especially triple-combination pills (like amlodipine + valsartan + HCTZ).
Research presented at the 2023 American Heart Association meeting showed patients on combo pills had 28% fewer hospitalizations for uncontrolled hypertension. That’s powerful.
But the biggest hurdle isn’t science. It’s access. Even if the pills exist, patients can’t use them if they’re too expensive, if insurance won’t cover them, or if their doctor doesn’t know they’re an option.
What Should You Do?
If you’re on multiple blood pressure pills:
- Ask your doctor: “Is there a combination generic I could switch to?”
- Check GoodRx or SingleCare for cash prices on the combo vs. separate pills.
- Call your insurance. Ask for the copay on both options.
- If the combo costs more and your insurance won’t budge, ask if you can get prior authorization.
- If you’re on a tight budget, stick with separate generics - but use a pill organizer.
If you’re just starting treatment:
- Ask your doctor if a combination pill is appropriate for your blood pressure level.
- Don’t assume the combo is automatically better - it’s better for adherence, not always for cost.
- Confirm the exact dose you need is available. Not all combinations come in all strengths.
Common Myths Debunked
- Myth: “Combination generics are less effective.”
Truth: They’re bioequivalent. They work just as well. - Myth: “I can’t get the dose I need.”
Truth: Some doses don’t exist. But many do. Ask for alternatives. - Myth: “Branded is better.”
Truth: 85% of prescriptions are generic. That’s because they work. - Myth: “I’ll save money by buying separate pills.”
Truth: Sometimes yes. Often no. Always check.
Final Thought
Antihypertensive combination generics aren’t magic. But they’re one of the most practical tools we have for controlling high blood pressure. They reduce confusion, cut costs over time, and save lives by helping people take their medicine.
They’re not perfect. Insurance policies are broken. Dosing options are limited. Access is unequal.
But if you’re taking two or three pills a day - and forgetting sometimes - switching to a single pill could be the simplest, most effective change you make this year.
Are combination blood pressure generics as effective as brand-name ones?
Yes. The FDA requires generic combination pills to meet strict bioequivalence standards - meaning they must deliver the same amount of medicine into your bloodstream as the brand-name version, within a 20% margin. Studies show they lower blood pressure just as effectively. The difference isn’t in effectiveness - it’s in cost and convenience.
Can I split a combination pill if I need a lower dose?
Only if the pill is scored (has a line down the middle). Some, like amlodipine/benazepril, are scored and can be split safely. Others aren’t. Never split a pill unless your pharmacist confirms it’s safe. Splitting can change how the drug is absorbed - especially if it’s a time-release formulation. If you need a specific dose that isn’t available in a combo, your doctor may need to prescribe the individual drugs separately.
Why does my insurance cover the separate pills but not the combo?
Insurance companies often have financial incentives to push separate generics. They may get rebates from manufacturers on individual drugs but not on combination pills. Even if the combo costs the pharmacy less, your copay might be higher because the insurer doesn’t consider it the most cost-effective option - even when it is for you. Always compare your copays for both options before deciding.
What if I need a dose that isn’t available in a combo pill?
Many standard doses are available - like 5mg/20mg or 10mg/40mg. But if you need, say, 2.5mg of amlodipine with 160mg of valsartan, that combo doesn’t exist. In that case, you’ll need to take the two pills separately. Your doctor can still help you manage it with a pill organizer or a medication app. Don’t settle for a dose that’s too high just because the combo doesn’t come in your needed strength.
Are triple-combination pills available as generics?
Yes, but they’re less common. Amlodipine/valsartan/hydrochlorothiazide is available as a generic in the U.S. and is growing in use. These are usually prescribed for patients who haven’t reached their target with two drugs. They’re more expensive than dual combos but can be cheaper than taking three separate pills. Availability varies by pharmacy and region.
Can I switch from a brand-name combo to a generic?
Yes, and most people do. Over 85% of combination antihypertensive prescriptions in the U.S. are generic. Switching is safe and common. Your doctor may need to write a new prescription, and your pharmacist will verify the generic is approved. Monitor your blood pressure for the first few weeks to make sure it stays controlled.

Dana Termini
January 7, 2026 AT 00:14Switched to amlodipine/valsartan last year after forgetting half my pills. My BP dropped from 160/98 to 124/80 in 6 weeks. No more pill organizer chaos. Just one pill, one time, done. Wish I’d done it sooner.
Lily Lilyy
January 8, 2026 AT 08:47It’s so important to remember that taking your medicine is not just about numbers on a screen-it’s about being there for your family, your friends, your future. One pill a day can mean years more with the people you love. Please don’t underestimate this simple change.
Susan Arlene
January 8, 2026 AT 20:33lol i thought combo pills were fancy brand stuff turns out theyre just 2 pills smashed together with a fancy label and 3x the price. my doc tried to push it but i just buy the two generics and put em in a pillbox. cheaper and i still remember to take em
Ashley S
January 9, 2026 AT 06:03Why do doctors even push these? It’s obvious they’re paid by pharma. I’ve seen people get sick from combo pills because they couldn’t adjust the dose. If you need different strengths, take separate pills. Don’t let them force you into a one-size-fits-all trap.
Jeane Hendrix
January 10, 2026 AT 08:56Just curious-has anyone tried comparing the bioequivalence data between specific generic combos and their brand-name counterparts? I’ve seen studies where the 80-125% range led to clinically significant variability in Cmax for certain subpopulations, especially in elderly patients with renal impairment. Would love to see the PK/PD breakdowns.
Rachel Wermager
January 10, 2026 AT 09:51Let’s be clear: the FDA’s bioequivalence standards are a joke. 80-125% AUC? That’s a 45% swing in systemic exposure. For a drug with a narrow therapeutic index like hydrochlorothiazide, that’s not ‘equivalent’-it’s a gamble. And don’t get me started on the lack of therapeutic drug monitoring for these combos. We’re treating hypertension like it’s a software update.
Leonard Shit
January 11, 2026 AT 04:34my pharmacist just handed me the combo pill and said ‘this one’s cheaper than buying them separate’… turned out he meant after my insurance denied the combo and covered the two generics at $5 each. i paid $48 for the combo. thanks, america.
Kelly Beck
January 12, 2026 AT 12:47YOU CAN DO THIS!! 💪 One pill a day is a small act of self-love. I was skeptical too-until I switched from three pills to one and my energy came back. My doctor said my BP is now ‘textbook perfect.’ You’re not just taking medicine-you’re reclaiming your life. Celebrate every day you take it! 🎉❤️
Wesley Pereira
January 13, 2026 AT 11:36insurance treats combo pills like they’re brand name even when they’re generic. why? because the rebate structure is broken. if you get the two generics, you’re saving $300/year. but if you take the combo? you’re paying $45 a month. so yeah, it’s not about science-it’s about corporate greed.
Isaac Jules
January 14, 2026 AT 08:37Anyone who takes these combos without checking their kidney function is playing russian roulette. Hydrochlorothiazide + ACEi = risk of hyperkalemia, acute kidney injury, especially in diabetics. You think it’s ‘just a pill’? Nah. It’s a chemical cocktail. Get labs done. Or don’t. But don’t act surprised when you end up in the ER.
Pavan Vora
January 15, 2026 AT 22:01In India, these combo pills are almost impossible to find in rural pharmacies. Even when available, the cost is 5x higher than in the US. Doctors here rarely prescribe them because they don’t know about them. WHO says 95% need them-but only 15% get them. This isn’t a health issue-it’s a justice issue.
Joann Absi
January 15, 2026 AT 23:06Why do Americans think they’re so special? In Europe, they’ve had these combos for decades. And they’re cheaper! And better regulated! We’re stuck in this capitalist nightmare where a pill that costs $10 abroad costs $40 here because of ‘patents’ and ‘pharma profits.’ Wake up.
Mukesh Pareek
January 16, 2026 AT 20:00Let me clarify the pharmacokinetics: Fixed-dose combinations are not inherently inferior, but the lack of individual titration capability renders them suboptimal for patients with comorbidities. The AUC variability between generics is not trivial-especially when combined with CYP3A4 inhibitors like grapefruit juice. You’re not just taking BP meds-you’re managing a metabolic ecosystem.
Brian Anaz
January 17, 2026 AT 23:21My cousin took a combo pill and had a stroke. His doctor didn’t check his electrolytes. Now he’s in a nursing home. Don’t be fooled. These pills are convenient, but they’re not safe for everyone. If your doctor pushes it without a full workup, find a new doctor.