Anticoagulants: Warfarin vs. DOACs - Safety, Side Effects, and What You Need to Know
 Nov, 14 2025
Nov, 14 2025
When your blood needs to thin - but not too much
Taking a blood thinner isn’t like taking a daily vitamin. One wrong move - a missed dose, a drug interaction, a fall - can send you to the ER. And with two main types of anticoagulants on the market, choosing the right one isn’t just about effectiveness. It’s about safety, daily life, and long-term risk.
For decades, warfarin was the only game in town. It worked, but it was finicky. You had to get your blood tested every few weeks, avoid spinach and kale, and double-check every new pill your doctor prescribed. Then came the DOACs - dabigatran, rivaroxaban, apixaban, edoxaban. No more weekly INR checks. No more dietary restrictions. Just pop a pill and go. But are they truly safer? And who still needs warfarin?
How warfarin works - and why it’s still around
Warfarin has been around since the 1950s. It blocks vitamin K, which your body needs to make clotting factors. Simple in theory, messy in practice. It takes 3 to 5 days to start working, and the dose varies wildly from person to person. One person might need 5 mg a day. Another might need 12 mg. That’s why regular INR blood tests are non-negotiable. Your target range? Between 2.0 and 3.0. Go above that, and you risk bleeding. Drop below, and clots form.
Over 300 drugs can interfere with warfarin. Antibiotics, painkillers, even some herbal supplements like St. John’s wort can throw your INR off. And food? Vitamin K-rich foods - broccoli, Brussels sprouts, spinach - can make warfarin less effective. It’s not that you can’t eat them. It’s that you have to eat the same amount every week. Consistency matters more than avoidance.
Still, warfarin isn’t obsolete. For people with mechanical heart valves, it’s the only option. DOACs don’t work here. They’ve been tested. They failed. The risk of valve clots and strokes is too high. Warfarin also stays the choice for patients with severe kidney failure (eGFR under 15). DOACs can build up in the body when kidneys can’t clear them, raising bleeding risk.
What DOACs are - and why they changed everything
Direct Oral Anticoagulants (DOACs) hit the scene in the 2010s and quickly became the new standard. Unlike warfarin, they don’t mess with vitamin K. Instead, they target specific clotting factors: dabigatran blocks thrombin (factor IIa), while apixaban, rivaroxaban, and edoxaban block factor Xa.
That’s why they’re predictable. Doses are fixed. No INR tests. No dietary restrictions. You take your pill at the same time every day - and that’s it. For most people, this is a game-changer. A 2023 JAMA Network Open study showed DOACs reduced the risk of recurrent blood clots by 34% compared to warfarin in people being treated for deep vein thrombosis or pulmonary embolism.
They’re also safer when it comes to brain bleeds. The American Heart Association found DOACs cut the risk of intracranial hemorrhage by about half. That’s huge. A brain bleed from a blood thinner is often fatal or disabling. Warfarin users have nearly twice the risk.
But not all DOACs are the same. Apixaban has the lowest bleeding risk among them. Rivaroxaban carries a slightly higher risk, especially in older or frail patients. Dabigatran has the lowest rate of recurrent clots but requires twice-daily dosing. Edoxaban is the least prescribed - partly because it’s newer and less familiar to doctors.
The safety trade-offs: DOACs aren’t perfect
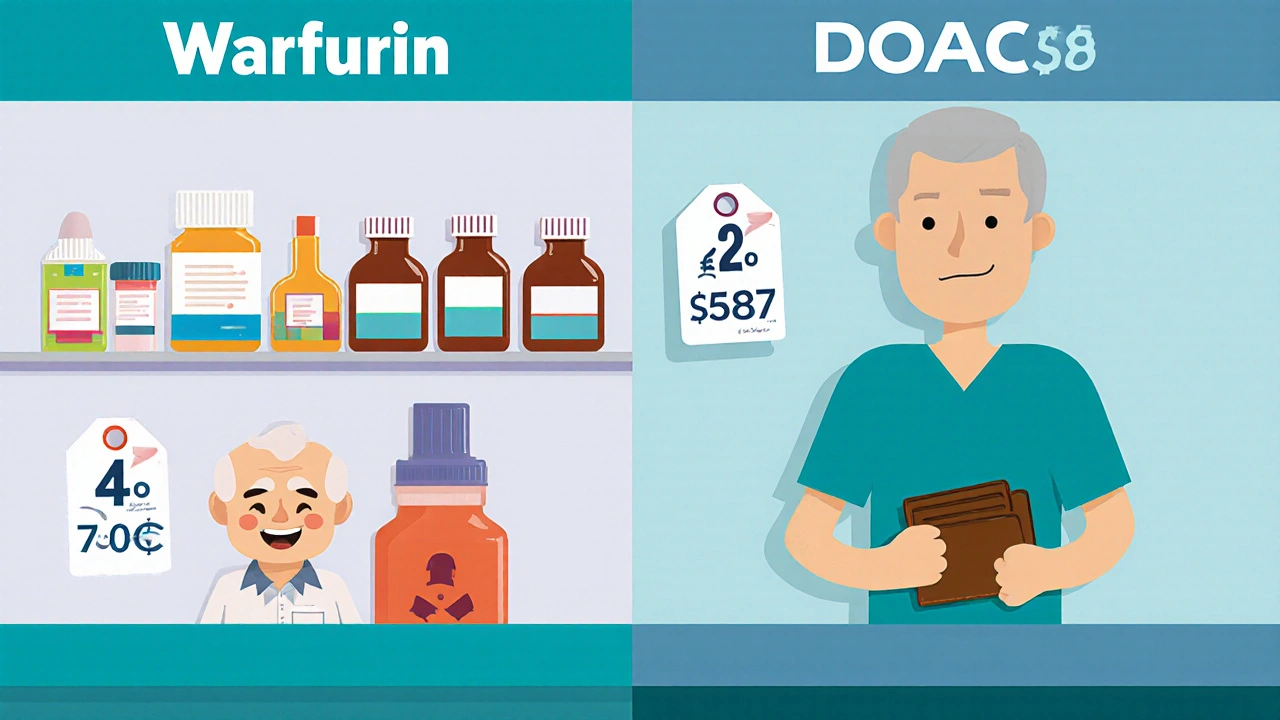
DOACs sound ideal - until they aren’t. First, cost. Warfarin costs about $4 a month. Apixaban? Around $587. Even with insurance, copays can hit $100 or more. That’s why some patients skip doses - or stop entirely. A 2023 study in the American Journal of Managed Care found DOAC users had 32% better adherence than warfarin users. But that gap shrinks when money is tight.
Second, kidney function. DOACs are cleared through the kidneys. Dabigatran? 80% cleared by kidneys. Apixaban? Only 27%. That means apixaban is safer for people with moderate kidney disease (eGFR 25-50). But if your eGFR drops below 25, even apixaban becomes risky. For patients on dialysis, guidelines still lean toward warfarin. There’s just not enough data to say DOACs are safe long-term in this group.
Third, reversal. If you bleed badly, you need a way to stop the anticoagulant fast. For warfarin, vitamin K and fresh frozen plasma work. For DOACs, you need specific reversal agents. Idarucizumab (Praxbind) reverses dabigatran. Andexanet alfa (Andexxa) reverses apixaban and rivaroxaban. These drugs are expensive and not always available in small hospitals. In an emergency, time matters. Waiting for a reversal agent can cost lives.
Who should stay on warfarin - and who should switch
Here’s the real-world breakdown:
- Switch to DOACs if: You have atrial fibrillation without a mechanical valve, no severe kidney disease, and can afford the medication. You want fewer blood tests and no dietary limits.
- Stay on warfarin if: You have a mechanical heart valve, severe kidney failure (eGFR <15), or you’re pregnant (DOACs are not safe in pregnancy). Also, if you’ve been stable on warfarin for years with good INR control, switching might not be worth the risk.
- Consider apixaban if: You’re older, have lower body weight, or have a history of bleeding. It’s the safest DOAC in these groups.
- Avoid rivaroxaban if: You’re over 75, have low body weight, or have moderate kidney issues. It carries the highest bleeding risk among DOACs.
Doctors now start nearly 9 out of 10 AF patients on DOACs. That’s up from just 1 in 3 in 2015. But that doesn’t mean warfarin is obsolete. It’s just more specialized now.
What patients actually say - real stories, real concerns
On patient forums, the split is clear. In a survey of over 1,200 people on Blood-Thinners.com, 78% preferred DOACs. Why? 89% cited no dietary restrictions. 82% loved not needing weekly blood tests.
But the warfarin users who stayed? They had reasons. One man, 82, said: “I’ve been on warfarin since my valve replacement in 2008. My INR’s been steady for 15 years. Why change?” Another woman, 67, said: “I can’t afford apixaban. My copay is $120. Warfarin is $5. I take it with my morning coffee. I know how it works.”
And then there’s the fear of forgetting. DOACs have a short half-life. Miss one dose? Your protection drops fast. Warfarin lingers longer. Miss a dose? You might still be protected for a day or two. That’s why adherence matters more with DOACs - and why some patients feel more secure with warfarin’s longer window.
What you should ask your doctor
If you’re on a blood thinner - or thinking about starting one - here’s what to ask:
- Do I have a mechanical heart valve or severe kidney disease? If yes, warfarin is likely still best.
- What’s my eGFR? If it’s under 30, DOACs may not be safe.
- Can I afford this? What’s my monthly copay? Are there patient assistance programs?
- Am I likely to miss doses? If yes, warfarin might be safer.
- Do I have a history of bleeding? Apixaban is the safest DOAC in that case.
- Is there a reversal agent available at my local hospital if I have a major bleed?
Don’t assume the newest drug is always best. The best drug is the one that fits your body, your life, and your budget.
What’s coming next
Research is moving fast. A new drug called Librexia™ - a combo of warfarin and vitamin K - is in phase 3 trials. The idea? Smooth out INR swings so patients don’t need as many tests. If it works, warfarin might make a comeback in a smarter form.
Another big study, AUGUSTUS-CKD, is comparing apixaban and warfarin in patients with advanced kidney disease and atrial fibrillation. Results are expected by late 2024. That could change guidelines for dialysis patients.
For now, the choice is clear: DOACs are safer and easier for most people. But warfarin still has its place - and for some, it’s the only safe option.

John Villamayor
November 15, 2025 AT 04:37Jenna Hobbs
November 16, 2025 AT 11:45Ophelia Q
November 17, 2025 AT 22:34Elliott Jackson
November 17, 2025 AT 22:50McKayla Carda
November 19, 2025 AT 00:31Christopher Ramsbottom-Isherwood
November 19, 2025 AT 05:26Stacy Reed
November 20, 2025 AT 17:35Robert Gallagher
November 22, 2025 AT 12:52Howard Lee
November 24, 2025 AT 06:05Nicole Carpentier
November 25, 2025 AT 16:21